Echolalia and echopraxia are two fascinating phenomena often encountered in individuals experiencing catatonia. These behaviors, characterized by the repetition of speech or actions, can be perplexing both for patients and those around them. While mimicry may seem like simple imitation, it plays a significant role in understanding communication challenges faced by these individuals.
Catatonia is more than just a symptom; it’s a complex state that affects behavior, movement, and emotional regulation. As we delve into the intricate world of echolalia and echopraxia within this context, we’ll explore their neurocognitive foundations, how they differ from other disorders, and their impact on social interaction. Understanding these aspects can illuminate pathways to effective treatment strategies that may enhance quality of life for those affected. Join us as we unravel the nuances behind these intriguing symptoms in catatonic states.
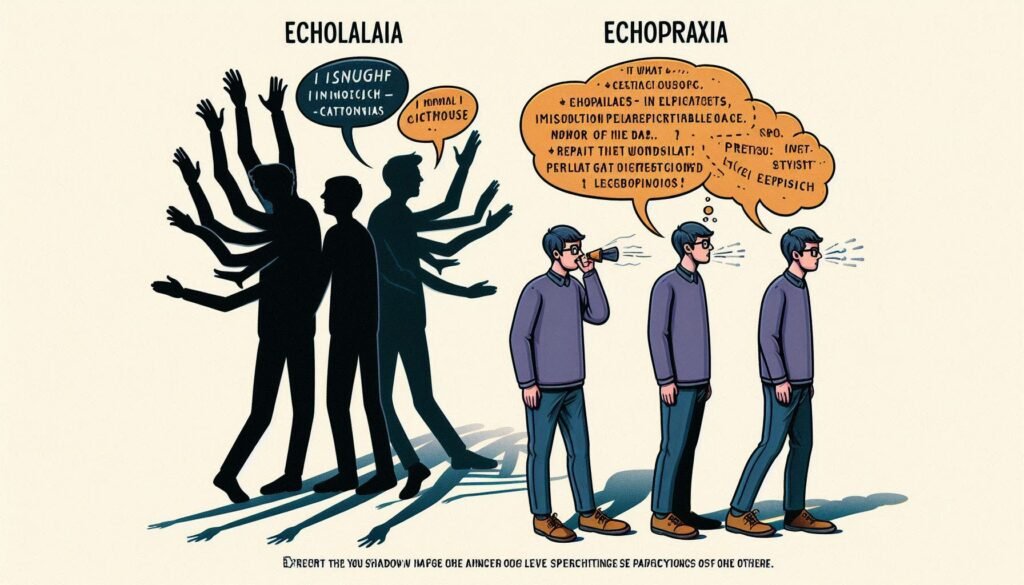
Defining Echolalia and Echopraxia: Mimicry Symptoms in Catatonia
Echolalia and echopraxia are two distinct yet related symptoms often observed in catatonia. Echolalia refers to the automatic repetition of words or phrases spoken by others, which can be immediate or delayed. This phenomenon can manifest as a means of communication when patients struggle to express themselves verbally.
On the other hand, echopraxia involves mimicking actions performed by others. This may include gestures, movements, or even whole sequences of behavior. Both symptoms reflect an underlying cognitive process where individuals exhibit involuntary mimicry rather than intentional imitation.
These behaviors serve as vital clues to understand how catatonia impacts communication skills and social interactions. While they might appear disconcerting at first glance, echolalia and echopraxia provide insight into the psychological state of affected individuals.
Recognizing these symptoms is essential for caregivers and healthcare professionals in tailoring appropriate interventions and support strategies for those experiencing catatonic states.
The Neurocognitive Basis of Echolalia and Echopraxia in Catatonic States
Echolalia and echopraxia in catatonic states stem from complex neurocognitive mechanisms. These phenomena involve the involuntary repetition of speech or actions, often reflecting underlying brain dysfunction. Research suggests that disturbances in areas such as the frontal lobes, basal ganglia, and limbic system play crucial roles.
Functional imaging studies have shown altered activity patterns during episodes of mimicry. This indicates a disconnection between intention and action, leading to automatic responses rather than conscious choices. Such disruptions can impair normal communication pathways.
The interplay between cognitive processing and motor functions is particularly significant in understanding these symptoms. When patients experience catatonia, their ability to generate spontaneous speech or purposeful movement becomes compromised. Instead, they resort to mimicking what they observe around them.
Understanding these neurocognitive underpinnings assists clinicians in diagnosing and managing catatonia more effectively. By recognizing echolalia and echopraxia as manifestations of deeper neurological issues, healthcare providers can tailor interventions accordingly.
Distinguishing Catatonic Echolalia from Other Speech Disorders
Catatonic echolalia is often mistaken for other speech disorders due to its mimicry of spoken language. Unlike typical echolalia, which may occur in autism or developmental delays, catatonic echolalia is specifically tied to a state of immobility or extreme agitation. Understanding this context is crucial for accurate diagnosis.
In catatonia, the repetition of words and phrases isn’t simply a reflex but can also reflect an emotional and cognitive shutdown. This differentiates it from conditions like verbal paraphasia or expressive aphasia, where patients struggle with language formulation rather than imitating speech they hear.
Clinicians must also consider that catatonic patients might exhibit limited spontaneous communication. Their echoic responses often lack the intent seen in other disorders. Furthermore, while patients with autism may use echolalic phrases meaningfully at times, those experiencing catatonia typically do not engage in reciprocal conversation.
Recognizing these distinctions aids mental health professionals in crafting tailored treatment plans and improving patient outcomes effectively.
Echopraxia in Catatonia: More Than Just Imitation
Echopraxia, often observed in catatonic patients, goes beyond mere imitation of actions. It involves the involuntary repetition or mimicry of another person’s movements. This behavior can manifest in various forms, from subtle gestures to more pronounced physical activities.
Unlike typical imitative behaviors seen in healthy individuals, echopraxia is a neurological symptom tied to underlying psychological conditions. In catatonia, this mimicry may stem from disrupted brain functions that impair voluntary motor control. The result can be an automatic response rather than a conscious choice.
The severity and context of echopraxia can vary significantly among patients. Some might mirror basic movements like hand gestures while others replicate complex sequences without awareness. These actions highlight deeper issues related to cognition and intention within these individuals.
Understanding echopraxia requires careful observation and insight into each patient’s unique condition. By analyzing their responses during interactions, caregivers can better tailor interventions for effective management and support.
The Spectrum of Mimicry: From Subtle to Pronounced Symptoms
Echolalia and echopraxia manifest on a spectrum, ranging from subtle to pronounced symptoms. In some cases, individuals may exhibit mild forms of mimicry that are easily overlooked. Subtle signs could include brief repetitions of words or phrases during conversation without an apparent intent to communicate.
As the condition intensifies, behaviors become more noticeable. Individuals might echo longer sentences or engage in more complex imitative actions. This escalation can lead to challenges in effective communication and social interactions.
In severe instances, patients may immerse themselves in repetitive speech patterns or compulsive mimicking of others’ movements. These pronounced symptoms disrupt everyday functioning and create barriers between the individual and their environment.
Understanding this spectrum is crucial for caregivers and healthcare professionals. It aids in recognizing the varying degrees of echolalia and echopraxia within catatonia, allowing for tailored interventions that address specific needs effectively.
Diagnostic Challenges: Identifying Echolalia and Echopraxia in Catatonia
Identifying echolalia and echopraxia in catatonia presents unique diagnostic challenges. Symptoms often overlap with other mental health disorders, making accurate assessment difficult. Clinicians must differentiate between primary catatonic symptoms and those attributed to conditions like autism or schizophrenia.
Echolalia can manifest as immediate repetition or delayed echoing of words, while echopraxia involves mimicking physical actions. This mimicry may appear intentional but is often involuntary, complicating the clinical picture further. Observers may misinterpret these behaviors without understanding their neurocognitive underpinnings.
Additionally, patients might display a range of communicative abilities that fluctuate over time. Some moments of clarity can lead to misconceptions about their overall condition when assessing speech patterns and movements.
Using standardized assessments alongside careful observation is essential in navigating these complexities. Collaboration among multidisciplinary teams provides a comprehensive view necessary for an accurate diagnosis tailored to each patient’s needs.
Impact on Communication and Social Interaction in Catatonic Patients
Echolalia and echopraxia significantly affect communication in catatonic patients. These conditions lead to repetitive speech or actions that can confuse interactions with others. When a patient mimics words or phrases without understanding, it hinders effective dialogue. Family members often struggle to engage meaningfully.
Social interaction is also impacted by these mimicry symptoms. The inability to respond appropriately can create awkwardness in social settings. Friends and loved ones may feel frustrated or concerned, feeling disconnected from the person they once knew.
In some cases, echolalia may evoke laughter or surprise, but this reaction isn’t always positive. It can perpetuate feelings of isolation for the patient when their responses don’t match the context of conversations.
Understanding these dynamics is essential for caregivers and therapists alike. Increased awareness fosters empathy and encourages more supportive environments for those struggling with these challenging aspects of catatonia.
Treatment Approaches: Addressing Echolalia and Echopraxia in Catatonia
Treatment for echolalia and echopraxia in catatonia often requires a multifaceted approach. Addressing the underlying causes is crucial, as these symptoms frequently arise from severe psychiatric conditions or neurological disorders. Psychotropic medications like antipsychotics may be employed to stabilize mood and reduce abnormal behaviors.
Behavioral therapies can also play a significant role. Techniques such as cognitive-behavioral therapy (CBT) aim to modify maladaptive thought patterns and improve functional communication skills. In structured environments, therapists can use modeling techniques to encourage more appropriate responses.
Occupational therapy may assist patients in developing daily living skills while enhancing their social interactions. This hands-on approach fosters independence, reducing reliance on mimicking behavior.
Family involvement is essential too. Education about echolalia and echopraxia helps families understand the condition better, which can lead to improved support at home. A collaborative effort between healthcare providers and families maximizes treatment effectiveness.
The Role of Therapy in Managing Repetitive Speech and Actions
Therapy plays a crucial role in managing echolalia and echopraxia in catatonic patients. It provides structured support to help individuals navigate their symptoms effectively. Tailored interventions can target the underlying causes of mimicry behaviors, fostering greater understanding and coping strategies.
Cognitive-behavioral therapy (CBT) is often utilized to reshape thought patterns related to repetitive speech and actions. This approach encourages patients to recognize triggers for their behaviors while developing healthier communication methods. Through guided practice, they can learn alternative ways to express themselves.
Additionally, occupational therapy focuses on enhancing daily living skills that may be impacted by these symptoms. Engaging patients in meaningful activities helps reduce reliance on mimicking behaviors while promoting independence and self-confidence.
Group therapy settings allow individuals with similar experiences to connect and share coping mechanisms. These interactions create a supportive environment where members feel understood, ultimately aiding their recovery journey through shared insights and encouragement from peers.
Prognosis and Long-Term Outcomes for Patients with These Symptoms
The prognosis for patients exhibiting echolalia and echopraxia in catatonia varies widely based on underlying causes, duration of symptoms, and individual response to treatment. Early intervention can significantly enhance outcomes. Many patients may experience a reduction or elimination of mimicry behaviors with appropriate therapeutic strategies.
Long-term effects often depend on the severity of the primary condition causing catatonia—such as schizophrenia or mood disorders—and whether those conditions are effectively managed. Some individuals regain functional communication skills and social interactions over time, while others may continue to struggle with persistent symptoms.
Ongoing support from mental health professionals is crucial. Tailored therapies focusing on communication skills can promote better engagement in daily activities. Family involvement plays a key role in recovery by providing emotional support and understanding.
Monitoring progress helps adapt treatment plans as necessary, ensuring that any emerging challenges are addressed promptly. With proper care and management, many individuals find ways to navigate their environments more successfully despite these complex symptoms associated with catatonia.


