Stereotypy in catatonia is a fascinating yet complex phenomenon that has intrigued mental health professionals and researchers alike. Characterized by repetitive movements or behaviors, it often manifests in individuals experiencing catatonic states—a condition typically marked by unresponsiveness or extreme agitation. Understanding the nuances of stereotypic movements can shed light on their implications for both diagnosis and treatment.
As we delve into this topic, we’ll explore what defines stereotypy in catatonia, its underlying neurobiological mechanisms, and how these seemingly simple motions carry significant meanings. Whether you’re a healthcare provider, caregiver, or simply curious about mental health conditions, grasping the intricacies of this subject can enhance your understanding of catatonia and improve outcomes for those affected. Join us as we unravel the layers behind stereotypy—its characteristics, impacts on daily life, diagnostic challenges—and effective strategies to manage these repetitive behaviors.
Defining Stereotypy in Catatonia: Characteristics and Types
Stereotypy in catatonia refers to the repetitive, non-functional movements or behaviors that often occur during catatonic episodes. These actions can range from simple gestures, such as hand flapping, to more complex sequences like pacing or rocking back and forth. While they may appear purposeless, these movements serve a significant role in the individual’s psychological state.
The characteristics of stereotypic movements include their consistency and persistence over time. Individuals may exhibit these behaviors for extended periods without variation. Such repetition can lead to physical exhaustion but also provides a form of self-soothing amidst distress.
Types of stereotypy vary widely among individuals experiencing catatonia. Some might engage in vocalizations or echolalia—repeating words or phrases they hear around them—while others display motor patterns like posturing or grimacing. Understanding these types is crucial for effective assessment and treatment planning.
Recognizing stereotypic behavior is essential for mental health professionals working with affected individuals. Proper identification helps differentiate between various psychiatric conditions and guides appropriate interventions.
The Neurobiological Basis of Stereotypic Movements in Catatonia
Stereotypy in catatonia is deeply rooted in neurobiological processes. Research indicates that these repetitive movements can stem from dysfunctions within the brain’s motor pathways. Specifically, abnormalities in regions such as the basal ganglia and frontal cortex play a crucial role.
The basal ganglia are essential for regulating voluntary movement. When disrupted, they may lead to abnormal patterns of behavior, including stereotypic movements seen in catatonic states. This suggests that neurotransmitter imbalances could trigger such behaviors.
Moreover, studies show that dopamine dysregulation significantly contributes to motor control issues. Elevated or diminished levels of this neurotransmitter can result in exaggerated or diminished responses to stimuli, leading to the repetition characteristic of stereotypy.
Understanding these neurobiological factors provides insight into why individuals with catatonia exhibit specific movement patterns. By exploring these mechanisms further, researchers hope to develop targeted interventions aimed at alleviating stereotypic behaviors associated with this complex condition.
Common Forms of Catatonic Stereotypy: From Simple to Complex
Catatonic stereotypy manifests in various forms, ranging from simple to complex behaviors. Simple movements often include repetitive gestures such as hand flapping, rocking back and forth, or pacing. These actions can appear almost rhythmic and serve as a way for individuals to cope with overwhelming feelings.
As we move toward more complex stereotypies, the behavior may involve intricate sequences of actions. For example, an individual might repeatedly arrange objects in specific patterns or engage in elaborate posturing that appears purposeless but is performed consistently.
These more complicated forms can sometimes be mistaken for purposeful activity due to their structured nature. However, they lack any real intention beyond repetition itself.
Understanding these distinctions is crucial for effective assessment and treatment strategies. Recognizing the spectrum of catatonic stereotypy helps caregivers tailor interventions that address both simple and complex manifestations appropriately.
Differentiating Catatonic Stereotypy from Other Repetitive Behaviors
Catatonic stereotypy presents unique characteristics that set it apart from other repetitive behaviors. While many individuals may engage in repetitive actions, the context and functions of these movements differ significantly in catatonia. Catatonic stereotypes often arise during periods of extreme immobility or withdrawal, reflecting a profound psychological state.
Contrastingly, other forms of repetitive behavior—like those seen in autism spectrum disorders or obsessive-compulsive disorder—typically serve different purposes. They might be used as coping mechanisms to alleviate anxiety or manage sensory overload rather than expressing an underlying catatonic state.
The intensity and persistence of movements also play a critical role in differentiation. Catatonic stereotypies can be more rigid and less responsive to external stimuli compared to other types of repetitive actions, which may vary based on environmental factors.
Recognizing these distinctions is vital for accurate diagnosis and treatment planning. Clinicians need to carefully assess the context and nature of the behavior for effective interventions tailored specifically for catatonia-related symptoms.
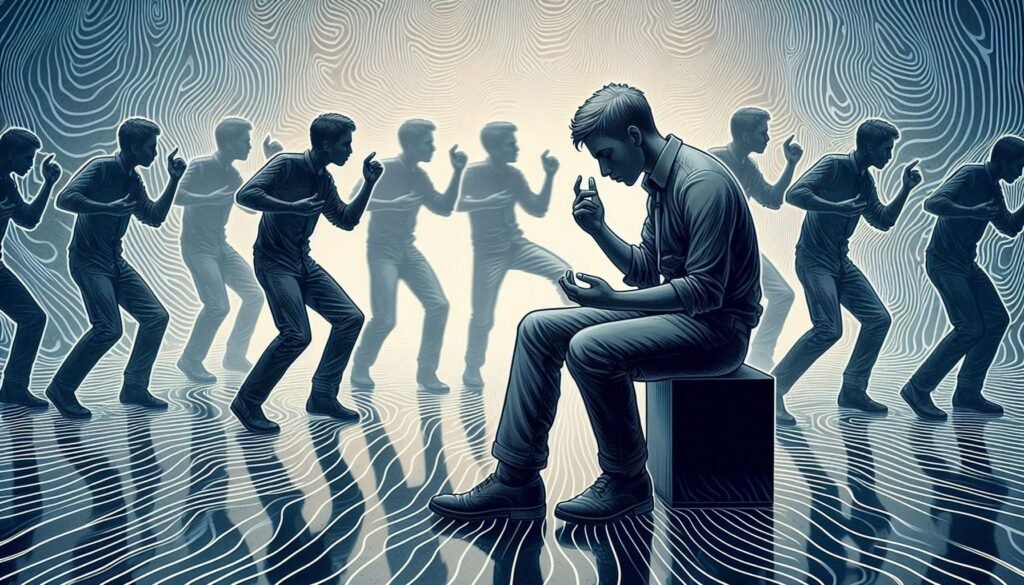
The Impact of Stereotypy on Daily Functioning and Quality of Life
Stereotypy in catatonia can significantly affect daily functioning. Individuals may find it challenging to engage in routine activities due to the repetitive movements that dominate their focus. These behaviors often consume time and energy, leading to neglect of personal care or responsibilities.
The impact extends beyond practical challenges. Those experiencing stereotypic movements may feel isolated from social interactions. Friends and family might struggle to understand these behaviors, resulting in strained relationships and heightened feelings of loneliness.
Quality of life is also compromised as individuals grapple with frustration stemming from an inability to control their actions. This lack of agency can lead to anxiety or depression, creating a vicious cycle that exacerbates the condition.
Moreover, environments such as workplaces or educational settings may become increasingly difficult for those exhibiting stereotypy. Disruptions caused by repeated movements can hinder participation in group tasks or collaborative efforts, further isolating affected individuals from meaningful experiences.
Assessing Stereotypy: Diagnostic Tools and Clinical Observations
Assessing stereotypy in catatonia requires a comprehensive approach. Clinicians often rely on both structured diagnostic tools and careful clinical observations to identify these repetitive movements. Standardized assessments, like the Catatonia Rating Scale, provide valuable insights into the frequency and nature of stereotypic behaviors.
Direct observation is equally important. Healthcare professionals watch for specific patterns, noting how long the movements last and their impact on daily activities. This qualitative data complements quantitative measures from rating scales.
Interviews with caregivers or family members can enhance understanding by revealing triggers or contexts that exacerbate stereotypy. These perspectives help paint a fuller picture of the individual’s experiences and challenges.
Integration of findings from various sources facilitates accurate diagnosis. By combining diagnostic tools with real-world observations, clinicians can develop effective treatment plans tailored to each patient’s needs.
Treatment Approaches: Managing Stereotypic Movements in Catatonia
Managing stereotypic movements in catatonia requires a multifaceted approach tailored to the individual’s needs. Treatment often starts with thorough assessment and diagnosis, as understanding the underlying causes is crucial for effective management. Once identified, mental health professionals can employ various strategies to address these movements.
Behavioral therapies play an essential role in treatment. These include techniques such as cognitive-behavioral therapy (CBT), which can help patients develop coping mechanisms and reduce anxiety linked to their symptoms. Engaging patients through structured activities may also diminish the frequency of stereotypies.
Medication is another cornerstone of treatment plans. Antipsychotic medications are commonly prescribed, targeting dopamine pathways that may contribute to these behaviors. In some cases, benzodiazepines or mood stabilizers might be used when appropriate.
Regular monitoring by healthcare providers ensures that treatments remain effective over time. Adjustments can be made based on patient response, leading to improved outcomes and enhanced daily functioning amidst challenges posed by stereotypy in catatonia.
Behavioral Interventions for Catatonic Stereotypy
Behavioral interventions play a crucial role in managing stereotypy in catatonia. These approaches focus on modifying specific behaviors to reduce the frequency and intensity of repetitive movements. Techniques can vary widely, but often emphasize positive reinforcement.
One effective method is prompting alternative behaviors. By encouraging individuals to engage in more functional activities during episodes of stereotypy, caregivers can help redirect attention away from repetitive actions. This redirection promotes engagement with their environment.
Another technique involves systematic desensitization. Gradually exposing individuals to triggers that prompt stereotypic behavior can help them develop coping strategies over time. This process requires patience and consistency from both therapists and family members.
Mindfulness practices also show promise as behavioral interventions for those experiencing catatonic stereotypy. Teaching individuals mindfulness techniques fosters awareness of their body movements, creating opportunities for self-regulation when they feel the urge to engage in repetitive motions.
The Role of Medication in Controlling Stereotypic Movements
Medication plays a crucial role in managing stereotypic movements associated with catatonia. Antipsychotic medications are often the first line of treatment. They target neurotransmitter imbalances that may contribute to these repetitive behaviors.
Benzodiazepines can also be effective, especially in cases where anxiety exacerbates symptoms. These medications help reduce agitation and promote relaxation, which may decrease the frequency of stereotypic movements.
In some instances, mood stabilizers or anticonvulsants are considered as adjunctive treatments. These drugs can address underlying mood disorders that might fuel catatonic symptoms, providing a more comprehensive approach to management.
It’s essential for healthcare providers to tailor medication plans individually. Regular monitoring is vital to assess effectiveness and adjust dosages accordingly, ensuring optimal outcomes for patients struggling with these challenging movements.
Long-Term Outcomes and Management of Stereotypy in Catatonia
Long-term management of stereotypy in catatonia requires a multifaceted approach that integrates behavioral therapy, medication, and ongoing assessment. Patients with catatonic symptoms often face challenges that can persist over time. Therefore, consistent support from healthcare providers is essential to improve their quality of life.
Research indicates that early intervention can lead to better outcomes. Behavioral strategies tailored to the individual’s needs can help reduce the frequency and intensity of stereotypic movements. Regular follow-up appointments allow clinicians to adjust treatment plans based on patient progress.
Medications such as antipsychotics or benzodiazepines may be effective for some individuals but should always be monitored closely due to potential side effects. A collaborative effort among psychiatrists, psychologists, and occupational therapists enhances the therapeutic environment.
Support groups also play a significant role in long-term management by providing emotional support and sharing coping strategies among peers facing similar challenges. As research into catatonia continues to evolve, staying informed about new findings will empower caregivers and families in managing this complex condition effectively. Ensuring a supportive atmosphere fosters resilience, enabling those affected by stereotypy in catatonia to thrive despite their struggles.


