Catatonia is a complex and often misunderstood condition that can profoundly impact an individual’s ability to function. Characterized by various motor, behavioral, and psychological symptoms, catatonia exists at the intersection of neurology and psychiatry. Understanding its neurobiological basis is crucial for developing effective treatments.
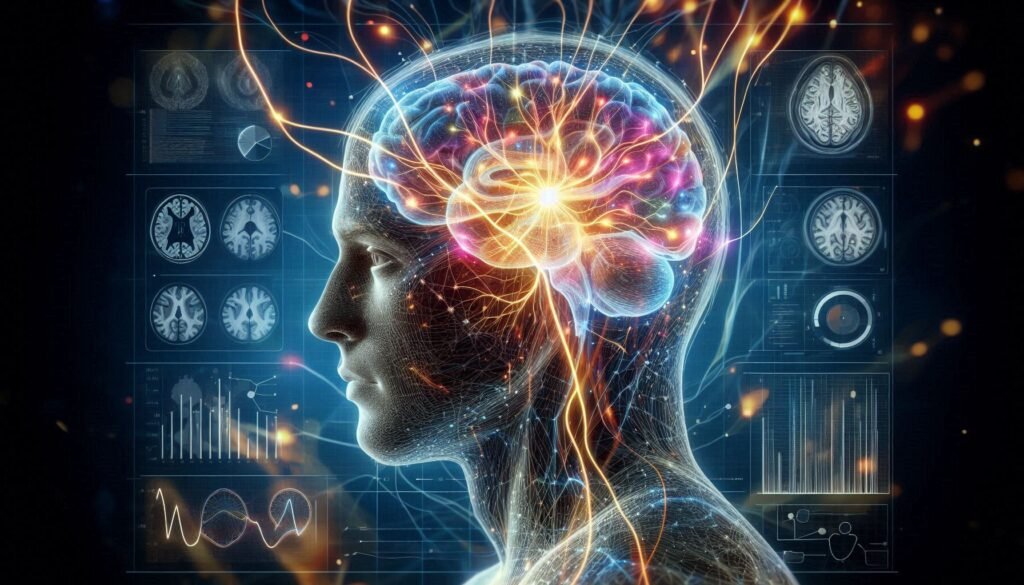
Recent research has shed light on the neural circuits involved in catatonic symptoms, revealing intricate relationships between different brain areas. As our knowledge expands, so too does our appreciation for how neurotransmitter imbalances contribute to this enigmatic state. By delving into brain imaging studies and exploring the roles of specific structures like the basal ganglia, we can better understand what happens neurologically during episodes of catatonia.
The exploration doesn’t stop there; factors such as neuroinflammation and genetic predispositions also play significant roles in shaping susceptibility to catatonic states. With advancements in neuroscience continuously unfolding before us, there’s hope for recovery through understanding neuroplasticity.
In this article, we’ll dive deep into these latest insights surrounding “The Neurobiological Basis of Catatonia,” equipping you with a comprehensive overview of how modern science interprets this puzzling condition.
Understanding Catatonia: A Brief Overview
Catatonia is a severe mental state that manifests primarily through abnormal motor behavior, ranging from immobility to excessive movement. It can occur in various psychiatric disorders, including schizophrenia and mood disorders, but it may also arise due to medical conditions or substance use.
People experiencing catatonia may exhibit symptoms such as stupor, mutism, echolalia, and even bizarre postures. These behaviors often perplex caregivers and healthcare professionals alike. Understanding the underlying mechanisms behind these symptoms is crucial for effective treatment.
Historically viewed as a rare phenomenon, recent studies indicate that catatonia is more prevalent than previously thought. Awareness of its clinical features has increased significantly over the years. The recognition of catatonia as a treatable condition marks an important shift in psychiatric care.
While some cases resolve quickly with appropriate interventions like benzodiazepines or electroconvulsive therapy (ECT), others can persist if left unaddressed. This highlights the need for ongoing research into the neurobiological factors driving this complex syndrome.
Neural Circuits Implicated in Catatonic Symptoms
Catatonia presents a complex array of symptoms that can significantly disrupt an individual’s functioning. Recent research highlights the crucial role of specific neural circuits in these manifestations. The interplay between various brain regions is essential for understanding how catatonic states arise.
One key area involved is the frontal cortex, which governs executive functions and voluntary movements. Disruptions here may lead to altered behavior and motor activity characteristic of catatonia. Additionally, connections between the prefrontal cortex and limbic structures appear to influence emotional expression and motivational drives.
The basal ganglia also play a pivotal part in regulating movement patterns. Dysfunction within this circuit can contribute to rigidity or immobility often seen in affected individuals. Moreover, interactions between the thalamus and other cortical areas are critical for processing sensory information, further complicating responses during catatonic episodes.
Identifying these neural circuits provides valuable insights into potential therapeutic approaches aimed at restoring normal function in those experiencing catatonia.
Neurotransmitter Imbalances in Catatonia
Neurotransmitter imbalances are thought to play a significant role in catatonia. Key neurotransmitters like dopamine, gamma-aminobutyric acid (GABA), and serotonin have been linked to its symptoms. Dopamine, in particular, is crucial for regulating motor control and emotional responses. Alterations in dopaminergic pathways may lead to the immobility or agitation observed in catatonic patients.
GABA serves as an inhibitory neurotransmitter that helps balance excitatory signals within the brain. Reduced GABA activity can result in heightened neuronal excitability, potentially contributing to the hyperactivity seen during episodes of catatonia. This imbalance can create a vicious cycle affecting overall mental state.
Serotonin also plays a pivotal role by influencing mood regulation and anxiety levels. Disruptions in serotonin levels might exacerbate feelings of despair or restlessness commonly associated with catatonia.
Research continues to explore how these neurotransmitter systems interact and contribute to the onset of catatonic symptoms, offering insights for potential therapeutic targets.
Brain Imaging Studies: Unveiling Structural Abnormalities
Recent advances in brain imaging techniques, such as MRI and PET scans, have significantly enhanced our understanding of the neurobiological basis of catatonia. These studies reveal critical structural abnormalities that may contribute to the manifestation of catatonic symptoms. For instance, researchers have observed reduced volumes in specific brain regions associated with motor control and emotional regulation.
The findings highlight alterations within areas like the prefrontal cortex and parietal lobes. These regions are crucial for decision-making and sensory processing. Their impairment can lead to the disorganized behaviors often seen in catatonic states.
Moreover, white matter integrity has shown correlations with symptom severity. Abnormalities in these neural pathways could hinder effective communication between different brain regions involved in motor planning and execution.
Brain imaging also sheds light on asymmetries that might be present between hemispheres during episodes of catatonia. Understanding these structural changes is vital for developing targeted interventions aimed at alleviating this complex disorder.
The Role of the Basal Ganglia in Catatonic States
The basal ganglia play a critical role in regulating movement and behavior, making them central to understanding catatonic states. This group of nuclei is intricately involved in motor control, emotional regulation, and cognitive functions. Disruptions within the basal ganglia can lead to the characteristic immobility or abnormal postures seen in catatonia.
Research suggests that abnormalities in dopamine pathways within the basal ganglia may contribute significantly to these symptoms. Dopamine dysregulation has been implicated not only in movement disorders but also in various psychiatric conditions associated with catatonia. The interplay between dopaminergic activity and other neurotransmitters may further exacerbate this state.
Moreover, alterations in connectivity among different regions of the basal ganglia could hinder effective communication necessary for normal functioning. Patients often exhibit rigidity or purposeless movements as a result of such dysfunctions.
Understanding how these neural circuits impact behavior opens avenues for potential therapeutic strategies aimed at restoring balance within this system. Targeting specific pathways might offer hope for those suffering from severe catatonic episodes.
Cortical Dysfunction and Catatonia: Exploring the Connection
Cortical dysfunction plays a crucial role in understanding the neurobiological basis of catatonia. The cerebral cortex is responsible for higher cognitive functions, including decision-making and emotional regulation. When this area malfunctions, individuals may exhibit symptoms characteristic of catatonia, such as unresponsiveness or abnormal postures.
Research has shown that disruptions in cortical activity can lead to impaired communication between different brain regions. This disconnection might exacerbate the rigid behaviors seen in catatonic states. Evidence suggests that specific areas within the cortex are particularly affected during episodes of catatonia.
Moreover, studies involving electroencephalography (EEG) have revealed altered electrical patterns in patients diagnosed with catatonia. These abnormalities indicate an underlying cortical dysfunction that could be pivotal for developing targeted treatments.
Understanding these connections not only sheds light on the experience of those suffering from catatonia but also opens avenues for therapeutic interventions aimed at restoring normal cortical function and improving patient outcomes.
Neuroinflammation and Its Impact on Catatonic Symptoms
Neuroinflammation plays a crucial role in the development and exacerbation of catatonic symptoms. This inflammatory response in the brain can disrupt normal neural functioning, leading to altered behavior and motor activity. The immune system’s activation may contribute significantly to these profound changes.
Research indicates that pro-inflammatory cytokines are often elevated in individuals experiencing catatonia. These molecules can influence neurotransmitter systems, particularly dopamine and glutamate pathways, which are essential for regulating mood and movement. When inflammation persists, it further complicates existing neurochemical imbalances.
Moreover, studies suggest that neuroinflammatory processes may lead to structural changes within key brain regions associated with motor control and emotional regulation. These alterations could manifest as rigidity or immobility characteristic of catatonia.
Understanding the relationship between neuroinflammation and catatonic symptoms is vital for developing targeted therapies. By addressing underlying inflammatory mechanisms, there is potential for improving treatment outcomes for affected individuals.
Genetic Factors Influencing Neurobiological Susceptibility
Genetic factors play a crucial role in determining an individual’s susceptibility to catatonia. Research indicates that specific gene variations may influence neurotransmitter systems, affecting how the brain responds to stress and environmental triggers. These genetic predispositions can create vulnerabilities that manifest as catatonic symptoms.
Studies have identified certain candidate genes associated with psychiatric disorders linked to catatonia, such as schizophrenia and mood disorders. Variations in genes related to dopamine regulation are particularly noteworthy. This connection highlights the importance of neurotransmitter activity in understanding the neurobiological basis of catatonia.
Moreover, familial patterns often emerge among those affected by this condition. Individuals with a family history of psychiatric illness may be at higher risk for developing catatonic states themselves, suggesting a heritable component worth investigating further.
Advancements in genomic research could pave the way for personalized treatment strategies targeting these genetic components. Understanding how genetics interplay with neurobiology will enhance our grasp of catatonia’s complexities and improve patient outcomes significantly.
Neuroplasticity in Catatonia: Potential for Recovery
Neuroplasticity refers to the brain’s ability to adapt and reorganize itself in response to experiences. This remarkable capacity may play a crucial role in understanding catatonia, particularly regarding recovery potential. Individuals experiencing catatonic symptoms often face significant challenges due to disruptions in their neural circuits.
Research suggests that targeted interventions can stimulate neuroplastic changes, promoting recovery from these debilitating states. For instance, therapies such as cognitive-behavioral therapy or physical rehabilitation might encourage new pathways for communication within the brain. These approaches aim not only at alleviating symptoms but also enhancing overall functioning.
Moreover, fostering an environment conducive to neuroplasticity—through social interactions and engaging activities—can be beneficial. Encouraging patients to participate in meaningful tasks helps strengthen existing networks while forming new connections.
Understanding how neuroplasticity operates within individuals with catatonia opens up exciting avenues for treatment strategies. By harnessing this natural adaptability of the brain, there is hope for improved outcomes and a greater quality of life for affected individuals.
Future Directions in Catatonia Neurobiology Research
As research progresses, the future of understanding the neurobiological basis of catatonia looks promising. Emerging studies are focusing on integrating various scientific disciplines, such as genetics and neuroimaging, to build a comprehensive framework for this complex disorder.
One exciting avenue is the exploration of targeted therapies that address specific neurotransmitter imbalances. Personalized medicine could revolutionize how we approach treatment for individuals experiencing catatonic symptoms. Additionally, advancements in brain imaging technologies may provide further insights into structural and functional abnormalities associated with catatonia.
Research is also delving deeper into genetic factors that predispose individuals to neurobiological vulnerabilities related to catatonia. Identifying these genes can lead to better risk assessment and early intervention strategies.
Furthermore, understanding neuroinflammation’s role opens new pathways for therapeutic interventions aimed at mitigating inflammatory responses in the brain.
Investigating how neuroplasticity can be harnessed for recovery offers hope. Rehabilitation strategies focusing on enhancing brain adaptability might improve outcomes for those experiencing catatonic states.
These future directions hold substantial potential not just to deepen our understanding but also to enhance care options available for patients dealing with this challenging condition.