Catatonia is a complex and often misunderstood condition that can leave patients, families, and even healthcare providers feeling perplexed. It manifests as a range of symptoms including immobility, mutism, and extreme withdrawal from the environment. While observation plays an essential role in identifying catatonia, it’s crucial to delve deeper into its underlying causes through laboratory testing.
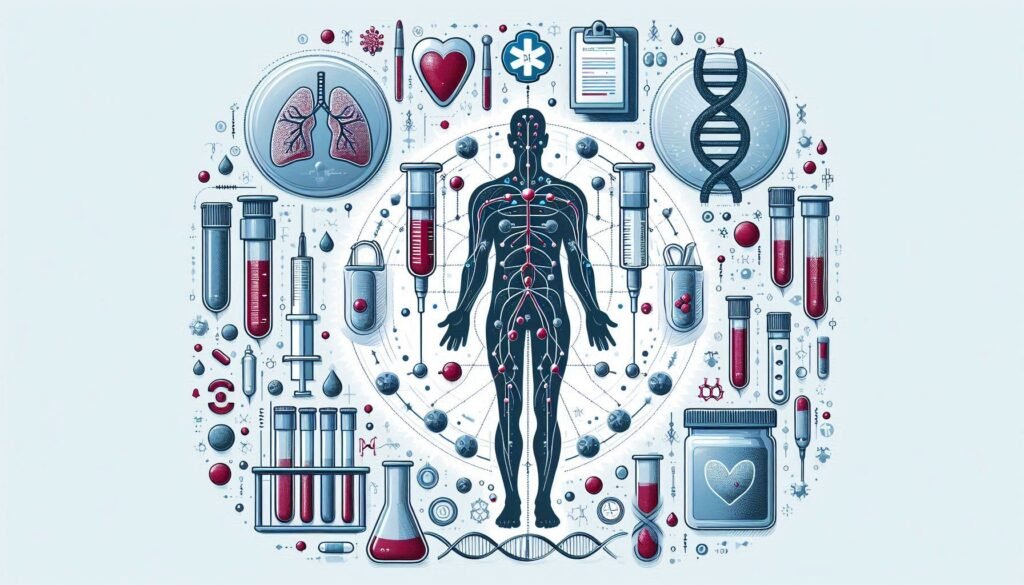
Essential laboratory tests for diagnosing underlying causes of catatonia can provide invaluable insights that lead to effective treatment strategies. By examining biological markers, clinicians can uncover hidden conditions such as metabolic disorders or autoimmune diseases that may contribute to a patient’s catatonic state. This comprehensive approach not only aids in accurate diagnosis but also opens up pathways for targeted interventions.
In this article, we will explore the pivotal role of various laboratory tests in diagnosing catatonia while shedding light on why these assessments are vital for optimal patient care. Whether you’re a clinician seeking knowledge or someone looking to understand more about this intricate disorder, read on to discover how these essential tests illuminate the path toward recovery.
The Importance of Laboratory Testing in Catatonia: A Comprehensive Approach
Laboratory testing plays a pivotal role in the comprehensive evaluation of catatonia. While clinical observation is essential, it often cannot pinpoint underlying medical issues that contribute to this complex condition. A thorough laboratory assessment can uncover hidden physiological disturbances.
Understanding catatonia requires more than just observing symptoms; it’s about identifying their causes. By utilizing various tests, healthcare providers gain critical insights into potential metabolic, infectious, or autoimmune factors at play. This multifaceted approach allows for tailored treatment plans.
Moreover, laboratory results can help differentiate between primary psychiatric disorders and secondary causes of catatonia. Recognizing these distinctions is vital for effective intervention and management strategies.
Timely laboratory testing also facilitates early diagnosis of potentially life-threatening conditions such as infections or electrolyte imbalances. In turn, prompt treatment may significantly improve patient outcomes and reduce the duration and severity of catatonic episodes.
Basic Blood Work: Complete Blood Count and Metabolic Panel in Catatonia Evaluation
Basic blood work is a crucial first step in evaluating catatonia. The Complete Blood Count (CBC) provides valuable insights into the patient’s overall health and can help identify infections or hematological abnormalities. For instance, elevated white blood cell counts may indicate an underlying infection that could contribute to catatonic symptoms.
The Metabolic Panel complements the CBC by assessing kidney function, electrolyte balance, and glucose levels. Abnormalities in these areas can lead to confusion or altered mental status, which may mimic or exacerbate catatonia. Low sodium levels, for example, might cause neurological disturbances requiring immediate attention.
These tests are quick and relatively simple but yield significant information about physical conditions affecting mental health. Timely identification of such factors is essential for effective treatment planning.
Basic blood work lays the groundwork for further diagnostic exploration while ensuring that any potential medical issues are addressed promptly.
Thyroid Function Tests: Uncovering Endocrine Causes of Catatonic Symptoms
Thyroid function tests are crucial in evaluating catatonia, particularly when endocrine issues may be at play. The thyroid gland regulates metabolism and energy levels through hormones such as T3 and T4. An imbalance can manifest in various mental health symptoms, including catatonia.
Hypothyroidism often presents with fatigue, depression, and cognitive dysfunction. These symptoms can mimic or contribute to catatonic states, making it essential for clinicians to assess thyroid hormone levels early in the diagnostic process. Elevated Thyroid-Stimulating Hormone (TSH) alongside low T3 and T4 indicates hypothyroidism.
Conversely, hyperthyroidism can lead to anxiety, agitation, and restlessness—factors that complicate an accurate diagnosis of catatonia. This condition is characterized by elevated levels of circulating thyroid hormones. Identifying these hormonal imbalances enables targeted treatment strategies tailored to the underlying cause.
By integrating thyroid function testing into the evaluation process for patients exhibiting catatonic symptoms, healthcare providers gain valuable insights that could significantly impact patient outcomes.
Autoimmune Markers: Identifying NMDA Receptor Encephalitis and Related Conditions
Autoimmune markers play a crucial role in diagnosing catatonia, particularly when NMDA receptor encephalitis is suspected. This condition often presents with psychiatric symptoms alongside neurological deficits. Identifying specific autoimmune antibodies can significantly enhance diagnostic accuracy.
Testing for NMDA receptor antibodies is essential. A positive result indicates the presence of an immune response targeting the receptors involved in regulating synaptic transmission and plasticity. The clinical presentation may include altered consciousness, agitation, and seizures, making laboratory testing vital.
In addition to NMDA receptor antibodies, other autoimmune markers should be considered. These include anti-GAD65 and anti-Ma2 antibodies that could suggest different underlying autoimmune processes. Understanding these conditions helps clinicians tailor treatment plans effectively.
Early detection through comprehensive testing improves patient outcomes dramatically. By addressing these autoimmune factors promptly, healthcare providers can initiate appropriate therapeutic interventions that address both the physical and mental aspects of catatonia.
Toxicology Screening: Ruling Out Substance-Induced Catatonia
Toxicology screening plays a crucial role in the evaluation of catatonia, particularly when considering substance-induced causes. Many psychoactive substances can mimic or exacerbate catatonic symptoms, making it essential to identify these factors early on.
Commonly tested substances include alcohol, benzodiazepines, opioids, and stimulants. These agents can lead to various degrees of sedation or agitation that may resemble classical catatonia. By conducting a thorough toxicology screen, clinicians can rule out these potential contributors.
Additionally, certain medications used for treating mental health disorders might also induce catatonic states as side effects. Identifying such medications is vital for appropriate management strategies tailored to each patient’s unique situation.
Understanding the influence of substances helps guide treatment decisions and offers patients a clearer path toward recovery. Addressing substance-related issues not only aids in diagnosis but also informs necessary interventions that target both the underlying cause and symptomatic relief.
Cerebrospinal Fluid Analysis: Insights from Lumbar Puncture
Cerebrospinal fluid (CSF) analysis is a crucial tool in evaluating catatonia. Obtained through a lumbar puncture, this procedure allows clinicians to examine the fluid that surrounds and protects the brain and spinal cord. Analyzing CSF can reveal important insights into underlying neurological conditions.
Elevated protein levels or abnormal cell counts may indicate infections, such as meningitis, or inflammatory diseases like autoimmune encephalitis. These findings can significantly impact treatment decisions for patients presenting with catatonic symptoms.
Additionally, specific tests on CSF can detect antibodies associated with conditions like NMDA receptor encephalitis. This particular condition has been linked to acute episodes of catatonia and requires prompt identification for effective intervention.
It’s essential for healthcare providers to consider CSF analysis as part of a comprehensive diagnostic approach when faced with unexplained catatonic behavior. The information gained from this procedure complements other laboratory tests, leading to more accurate diagnoses and tailored treatments.
Genetic Testing: Exploring Hereditary Factors in Catatonia
Genetic testing plays a crucial role in understanding the hereditary factors that may contribute to catatonia. Certain genetic mutations can predispose individuals to psychiatric disorders, including conditions that manifest with catatonic features. By analyzing a patient’s family history and identifying potential genetic links, clinicians can tailor their diagnostic approach.
Next-generation sequencing technologies allow for comprehensive evaluations of multiple genes simultaneously. This method not only identifies known variants but also uncovers novel mutations associated with catatonia. Such insights help distinguish between primary psychiatric causes and those arising from underlying genetic syndromes.
Additionally, exploring specific gene panels related to neurotransmitter systems or neurodevelopmental pathways enhances our understanding of how genetics may influence behavior and brain function in these patients. These findings could lead to targeted interventions or preventive strategies for at-risk individuals.
As research continues, the integration of genetic information into clinical practice will become increasingly important. Enhanced awareness will aid healthcare providers in making informed decisions regarding diagnosis and treatment options for patients experiencing catatonia.
Inflammatory Markers: C-Reactive Protein and Erythrocyte Sedimentation Rate
Inflammatory markers like C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR) play a crucial role in evaluating catatonia. These tests help identify underlying inflammatory processes that may contribute to the condition. Elevated levels of CRP indicate acute inflammation, often signaling infection or autoimmune disorders.
The ESR test measures how quickly red blood cells settle at the bottom of a test tube over one hour. A higher rate suggests systemic inflammation, which could be related to various medical conditions affecting neurological function. In cases of catatonia, elevated ESR can hint at an underlying process requiring further investigation.
Both CRP and ESR are non-specific indicators; however, their results can guide clinicians toward more targeted diagnostic testing. Identifying these inflammatory responses is key for developing an effective treatment plan tailored to each patient’s unique situation.
Monitoring these markers over time can also provide insight into treatment efficacy and disease progression, making them invaluable tools in managing catatonic symptoms.
Vitamin Deficiency Tests: B12, Folate, and Vitamin D in Catatonia
Vitamin deficiencies can significantly impact neurological health. In the context of catatonia, testing for levels of Vitamin B12, folate, and Vitamin D becomes crucial. These vitamins play vital roles in brain function and mood regulation.
Vitamin B12 is essential for nerve health and cognitive functions. A deficiency may lead to neuropsychiatric symptoms such as confusion or altered mental status—potentially mimicking catatonic states. Folate is equally important; low levels can result in similar cognitive impairments that could complicate a diagnosis.
Vitamin D has emerged as a player in mental health too. Deficiency has been linked with various psychiatric conditions, including depression and psychosis. Its role in modulating immune response may also influence inflammatory processes tied to catatonia.
Testing these vitamin levels provides valuable insights into underlying causes of catatonia. Identifying deficiencies allows clinicians to address them appropriately, ensuring comprehensive care tailored to each patient’s needs.
Interpreting Laboratory Results: A Guide for Clinicians Diagnosing Catatonia
Interpreting laboratory results in the context of diagnosing catatonia requires a meticulous approach. Clinicians must integrate findings with clinical observations and patient history for accurate diagnosis. Each test offers critical insights into potential underlying causes, whether metabolic, autoimmune, or infectious.
When reviewing results from basic blood work, it’s essential to consider abnormalities that could signal systemic issues. For instance, a complete blood count revealing leukocytosis might indicate an infection contributing to catatonic behavior. Similarly, fluctuations in electrolyte levels on a metabolic panel could point towards dehydration or renal dysfunction.
Thyroid function tests can elucidate endocrine disorders that mimic psychiatric symptoms; hyperthyroidism may present similarly to mania while hypothyroidism might induce significant lethargy and cognitive impairment.
Autoimmune markers require careful evaluation as well. A positive NMDA receptor antibody could lead clinicians toward an encephalitis diagnosis rather than primary psychiatric illness.
Moreover, toxicology screenings are crucial for ruling out substance-induced cases of catatonia—substance use can easily complicate presentations and treatment strategies.
Genetic testing may reveal hereditary factors influencing susceptibility to various forms of catatonia. By comprehensively understanding these lab results through collaborative interpretation with specialists when needed, clinicians can provide targeted care plans tailored to each patient’s unique needs and underlying conditions related to their catatonic state.