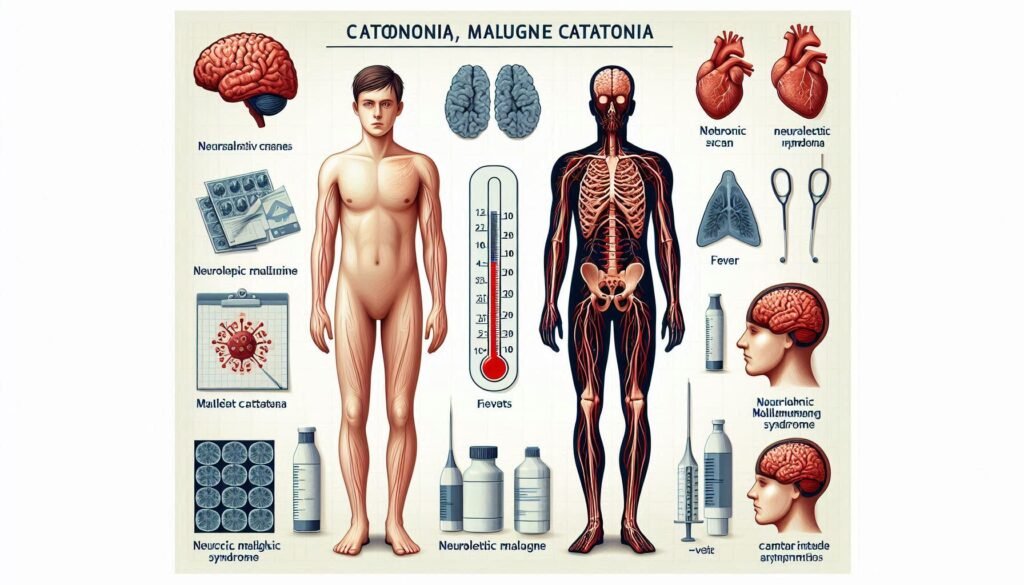
When it comes to severe psychiatric conditions, two disorders often create confusion due to their overlapping symptoms: Malignant Catatonia (MC) and Neuroleptic Malignant Syndrome (NMS). Both can present as life-threatening emergencies, making accurate diagnosis crucial. Misidentifying one for the other could have dire consequences for patient care.
The clinical worlds of MC and NMS are intricate yet fascinating. Understanding how they intersect while also recognizing their distinct features is essential for healthcare professionals. With proper differentiation, we pave the way towards effective treatment strategies that can save lives.
In this article, we will explore various aspects that help in differentiating Malignant Catatonia from Neuroleptic Malignant Syndrome. From symptom progression and medication history to laboratory findings and neuroimaging insights, each section aims to provide clarity on these complex disorders. Join us as we delve into a nuanced understanding that every clinician should embrace in order to make informed decisions under pressure.
Understanding the Overlap: Malignant Catatonia and NMS Similarities
Malignant Catatonia (MC) and Neuroleptic Malignant Syndrome (NMS) share several alarming similarities, often complicating clinical diagnosis. Both disorders can arise abruptly, usually in response to significant stressors or medication changes. This sudden onset makes it critical for healthcare providers to act quickly.
Both conditions are characterized by severe motor disturbances. In MC, these may manifest as extreme rigidity and bizarre posturing. NMS presents similarly but is typically associated with the use of antipsychotic medications that disrupt dopamine pathways.
Another commonality lies in autonomic dysfunction. Patients experiencing either condition may exhibit fluctuating vital signs, including elevated heart rates and blood pressure changes. Such instability can pose immediate risks if not promptly addressed.
Both MC and NMS can lead to altered mental status ranging from confusion to complete unresponsiveness. Recognizing these overlaps is essential for clinicians navigating the complexities of differential diagnosis in urgent care settings.
Clinical Presentation: Key Differences in Symptom Progression and Severity
Malignant Catatonia (MC) and Neuroleptic Malignant Syndrome (NMS) can present with similar symptoms, but their progression and severity often differ significantly. MC typically starts with a marked change in motor behavior, such as stupor or extreme agitation. Patients may exhibit odd posturing or waxy flexibility early on.
In contrast, NMS usually begins after exposure to antipsychotic medications. Symptoms like hyperthermia, muscle rigidity, and autonomic instability often follow within days of initiating treatment. The onset is more abrupt compared to the gradual development seen in MC.
When it comes to severity, MC can manifest profound psychological effects alongside physical symptoms—delirium is common. In contrast, NMS primarily features severe neurologic dysfunction without these significant changes in mental status.
Monitoring symptom evolution is crucial for accurate diagnosis. Recognizing how quickly and intensely each condition develops aids healthcare providers in differentiating between these potentially life-threatening syndromes.
Medication History: The Role of Antipsychotics in Differential Diagnosis
Medication history plays a crucial role in differentiating malignant catatonia from neuroleptic malignant syndrome (NMS). Understanding a patient’s recent exposure to antipsychotics can provide vital clues. Malignant catatonia often arises in response to stress or medical conditions, but it may also emerge after the abrupt withdrawal of certain medications.
In contrast, NMS is frequently linked directly to the use of antipsychotic drugs. Patients with NMS usually present shortly after starting or increasing their dosage of these medications. Identifying any changes in treatment regimens helps clinicians assess the likelihood of either condition.
Furthermore, even if both disorders involve severe muscle rigidity and altered mental status, knowing when symptoms developed relative to medication adjustments can aid in diagnosis. For example, if symptoms commenced within days of an antipsychotic increase, NMS becomes more probable.
Careful evaluation of medication history not only informs diagnosis but also guides appropriate treatment strategies for affected individuals. Recognizing this aspect is essential for effective patient care.
Laboratory Findings: Distinguishing Biomarkers in MC and NMS
Laboratory findings play a crucial role in differentiating malignant catatonia (MC) from neuroleptic malignant syndrome (NMS). Both conditions can present with elevated creatine kinase levels, but the underlying causes differ significantly. In NMS, this elevation is often attributed to muscle rigidity and breakdown due to neuroleptic medication.
In contrast, MC may also exhibit increased creatine kinase; however, it typically arises from prolonged immobility or severe agitation rather than medication effects alone. Moreover, electrolyte imbalances are common in both conditions but serve as additional markers for diagnosis.
Other laboratory tests can reveal leukocytosis and metabolic acidosis alongside elevated liver enzymes in some patients with NMS. These findings further accentuate the biochemical stress associated with this syndrome.
Conversely, MC may show signs of autonomic dysregulation through distinct laboratory profiles like variations in cortisol levels. Such differences highlight the importance of targeted testing when distinguishing between these complex syndromes.
Neuroimaging Insights: Brain Patterns in Malignant Catatonia vs. NMS
Neuroimaging studies play a crucial role in differentiating malignant catatonia (MC) from neuroleptic malignant syndrome (NMS). Recent advancements in techniques like MRI and PET scans have unveiled distinct brain patterns associated with each condition.
In malignant catatonia, abnormalities often emerge in the frontal lobes and basal ganglia. These areas are pivotal for motor control and cognitive functions. Imaging may reveal hyperactivity or atrophy, suggesting an underlying dysfunction that drives the severe psychomotor disturbances characteristic of MC.
Conversely, NMS typically showcases changes linked to dopaminergic pathways affected by antipsychotic medications. Neuroimaging might illustrate alterations in subcortical structures that correlate with muscle rigidity and autonomic dysregulation seen in this syndrome.
By analyzing these imaging findings alongside clinical symptoms, healthcare providers can make more informed decisions about diagnosis and treatment strategies. This highlights the importance of precise neuroimaging in understanding these complex conditions better.
Treatment Response: Diagnostic Clues from Intervention Outcomes
Treatment response can provide critical insights when differentiating malignant catatonia from neuroleptic malignant syndrome. Each condition typically reacts distinctively to different therapeutic approaches, offering clues for accurate diagnosis.
Patients with malignant catatonia often show a favorable response to benzodiazepines and electroconvulsive therapy (ECT). Rapid improvement in psychomotor agitation or stupor can suggest that the underlying issue is catatonia rather than NMS. This swift reaction serves as an essential marker in clinical settings.
On the other hand, neuroleptic malignant syndrome usually necessitates discontinuation of antipsychotic medications. Intravenous fluids and supportive care are crucial here, but recovery might take longer compared to malignant catatonia treatment outcomes.
Monitoring how each patient responds not only aids diagnosis but also directs ongoing management strategies. A careful examination of these responses helps clinicians differentiate between these life-threatening conditions effectively.
Time Course and Onset: Temporal Differences Between MC and NMS
The time course and onset of malignant catatonia (MC) and neuroleptic malignant syndrome (NMS) can be quite distinct. MC typically presents gradually, often developing over days to weeks. It may start with subtle signs such as agitation or extreme anxiety before evolving into more severe symptoms.
In contrast, NMS usually manifests acutely within hours to a few days after the administration of antipsychotic medications. Patients might experience an abrupt increase in muscle rigidity, fever, and autonomic instability soon after exposure to these drugs. This rapid progression can make NMS particularly dangerous if not recognized early.
Moreover, the duration of symptoms also differs between the two conditions. While MC may have a fluctuating course with potential episodes of remission, NMS tends to maintain its severity until appropriate treatment is initiated.
Understanding these temporal differences is crucial for clinicians aiming to make accurate diagnoses and intervene promptly in either condition. Recognizing when symptoms began can guide further investigation into the patient’s history.
Autonomic Instability: Comparing Patterns in MC and NMS
Autonomic instability is a significant feature that can differentiate malignant catatonia (MC) from neuroleptic malignant syndrome (NMS). Both conditions present with alterations in autonomic function, but the patterns often diverge.
In MC, patients may exhibit bizarre behavioral changes alongside symptoms like hyperthermia and fluctuating blood pressure. The autonomic dysregulation tends to be more erratic, reflecting the complex interplay of psychological stressors and physiological responses.
On the other hand, NMS typically shows more consistent autonomic signs. Patients usually experience stable fever spikes and pronounced muscle rigidity leading to increased sympathetic activity. This often results in predictable cardiovascular instability, such as tachycardia or bradycardia.
Understanding these differences helps clinicians assess patient presentations accurately. Recognizing whether one condition presents with erratic versus stable autonomic features can guide effective management strategies tailored to each diagnosis.
Muscle Rigidity and Movement Disorders: Subtle Distinctions
Muscle rigidity is a hallmark symptom in both Malignant Catatonia (MC) and Neuroleptic Malignant Syndrome (NMS), yet the characteristics of this rigidity can vary significantly. In MC, patients often exhibit a peculiar form known as “waxy flexibility.” This means their limbs may remain in any position they are placed, reflecting an unusual resistance to passive movement.
Conversely, NMS typically presents with more pronounced muscle rigidity. Patients experience severe stiffness that affects the entire body and is often accompanied by tremors or abnormal posturing. The intensity of this rigidity can lead to complications like rhabdomyolysis if not addressed promptly.
Movement disorders also differ between these conditions. Individuals with MC may demonstrate marked psychomotor retardation, where voluntary movements become noticeably slowed or absent altogether. In contrast, those suffering from NMS might display irregularities such as akinesia or catatonia-like states due to neuroleptic medications.
Recognizing these subtle distinctions is crucial for healthcare providers tasked with differentiating between these life-threatening syndromes effectively.
Diagnostic Algorithms: Systematic Approaches to Differentiating MC from NMS
Diagnostic algorithms play a crucial role in differentiating malignant catatonia (MC) from neuroleptic malignant syndrome (NMS). These systematic approaches are designed to streamline the diagnostic process, ensuring timely and accurate identification of each condition.
Clinicians often employ flowcharts that incorporate clinical symptoms, medication history, and laboratory findings to guide their assessments. For instance, an algorithm may begin with assessing motor functions—muscle rigidity or movement disorders are common indicators for both MC and NMS but require careful evaluation against other markers.
Next, these algorithms emphasize the importance of patient history regarding antipsychotic use. Recognizing prior exposure can rapidly narrow down potential diagnoses. Laboratory tests measuring creatine kinase levels and electrolyte imbalances further aid in distinguishing between these two severe conditions.
Utilizing such structured methodologies helps prevent misdiagnosis while facilitating effective treatment pathways tailored to the specific needs of patients experiencing either MC or NMS. The implications of accurate differentiation cannot be overstated; it is vital for improving outcomes and reducing mortality associated with these life-threatening lookalikes.