Catatonia is a complex neuropsychiatric condition that can leave patients in a state of extreme agitation or immobility. Treating catatonia often requires more than just one approach; it demands an innovative strategy to address its multifaceted symptoms. That’s where combination therapies come into play.
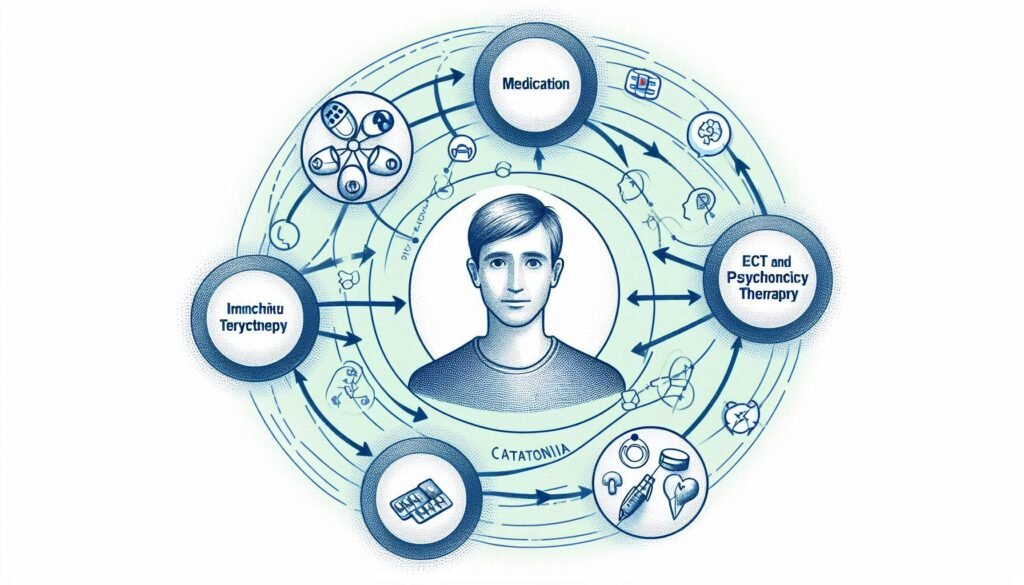
These synergistic treatment strategies blend various therapeutic modalities, harnessing their strengths to create a comprehensive care plan tailored for each individual. From pharmacological options to psychotherapy and even nutritional support, the potential for combining treatments offers hope for enhanced efficacy and improved patient outcomes.
In this blog post, we will delve into the rationale behind these combination therapies in catatonia treatment and explore how integrating different methods can lead to better results while minimizing side effects. Let’s embark on this journey through the evolving landscape of catatonia management together!
The Rationale Behind Combination Therapies in Catatonia Treatment
Catatonia presents a unique challenge due to its varied symptoms and underlying causes. Traditional treatments may not address the complexity of each patient’s experience, leading to a need for more nuanced approaches. Combination therapies allow clinicians to tackle multiple dimensions of the disorder simultaneously.
One key rationale is that different treatment modalities can target specific symptoms that arise in catatonia. For instance, while some patients may experience severe motor disturbances, others might struggle with mood or anxiety issues. By integrating various strategies, healthcare providers can implement tailored solutions.
Additionally, using combinations can enhance overall treatment efficacy. Certain medications complement each other by amplifying therapeutic effects while potentially reducing side effects associated with higher doses of single agents.
Furthermore, combining pharmacological interventions with psychosocial therapies addresses both biological and psychological components of catatonia. This holistic perspective fosters better engagement from patients and promotes recovery through multifaceted support systems designed specifically for their needs.
Pharmacological Combinations: Enhancing Efficacy and Reducing Side Effects
Pharmacological combinations are increasingly recognized as a potent strategy in treating catatonia. By utilizing two or more medications, clinicians can enhance treatment efficacy while minimizing the risk of side effects. This approach allows for targeting multiple pathways involved in this complex condition.
For instance, combining antipsychotics with mood stabilizers may address both psychotic symptoms and mood dysregulation simultaneously. Such synergistic effects often lead to improved patient outcomes when compared to monotherapy. Adjusting dosages carefully is crucial to achieving optimal results without overwhelming the patient’s system.
Moreover, some pharmacological combinations can counteract undesirable side effects associated with individual drugs. For example, certain antidepressants might alleviate sexual dysfunction caused by antipsychotics, thus improving adherence to treatment plans.
The careful selection of these drug combinations is essential in tailoring therapies that suit specific patient profiles. Clinicians must be vigilant about potential interactions and adjust treatments accordingly for safe and effective management of catatonia.
Integrating Pharmacotherapy with ECT: A Powerful Dual Approach
Electroconvulsive therapy (ECT) has long been recognized as an effective intervention for severe mood disorders and catatonia. When combined with pharmacotherapy, this dual approach can significantly enhance treatment outcomes. ECT often alleviates acute symptoms more rapidly than medications alone, providing immediate relief.
Pharmacotherapy plays a critical role in maintaining stability after ECT sessions. Antidepressants or antipsychotics can help sustain the therapeutic effects achieved through ECT while preventing relapse of catatonic symptoms. This synergy is especially beneficial in patients who experience recurrent episodes.
Moreover, using both modalities allows clinicians to tailor treatments based on individual patient needs. For instance, adjusting medication dosages post-ECT can optimize recovery while minimizing side effects.
It’s essential that healthcare providers monitor patients closely during this integrated treatment process to ensure safety and efficacy. By blending these powerful therapies, practitioners can offer a more comprehensive care plan for individuals experiencing the complexities of catatonia.
Combining Benzodiazepines with NMDA Antagonists: Mechanism and Benefits
Benzodiazepines and NMDA antagonists represent an intriguing combination in treating catatonia. Benzodiazepines primarily work by enhancing GABA activity, leading to sedation and anxiolytic effects. This can be crucial for patients experiencing severe agitation or anxiety associated with catatonic states.
On the other hand, NMDA antagonists like ketamine block glutamate receptors, which may help alleviate symptoms of depression and psychosis often present in these patients. By targeting different neurotransmitter systems, this combination can address multiple facets of catatonia simultaneously.
The synergy between these two classes of drugs may lead to a more rapid response compared to monotherapy. Furthermore, benzodiazepines might mitigate some side effects commonly associated with NMDA antagonists, such as dissociative symptoms.
This dual approach not only enhances therapeutic efficacy but also provides a broader safety net for managing complex cases. Clinicians are increasingly considering this strategy when developing individualized treatment plans for their patients battling catatonia.
Psychotherapy as an Adjunct to Biological Treatments in Catatonia
Psychotherapy can play a vital role in the treatment of catatonia, complementing biological interventions. While medications and ECT are often the first line of defense, integrating psychotherapy can enhance recovery outcomes. It offers patients emotional support and coping strategies that medications alone may not provide.
Cognitive-behavioral therapy (CBT) is particularly beneficial. It helps individuals understand their thoughts and feelings surrounding their catatonic experiences. This understanding can reduce anxiety and promote engagement with both therapeutic processes and daily activities.
Additionally, supportive psychotherapy encourages expression without judgment, fostering a safe environment for patients to process their emotions. This therapeutic alliance may also bolster motivation to adhere to medical treatments.
Moreover, incorporating family therapy can address interpersonal dynamics that contribute to stress or trauma within familial relationships—factors often exacerbating symptoms of catatonia. By harnessing these psychotherapeutic tools alongside pharmacological treatments, clinicians can create a more comprehensive approach tailored to individual needs.
Nutritional Supplementation in Conjunction with Standard Therapies
Nutritional supplementation plays a vital role in the comprehensive treatment of catatonia. Many patients experience nutritional deficiencies due to their condition, which can exacerbate symptoms and hinder recovery. Addressing these gaps through supplements can provide essential nutrients that support brain health and overall well-being.
Certain vitamins, such as B12 and D, are particularly important for mood regulation and cognitive function. Omega-3 fatty acids have also shown promise in reducing inflammation within the brain, potentially alleviating some catatonic symptoms. Additionally, magnesium has been linked to improved neurotransmitter function and may help ease anxiety.
Incorporating these supplements alongside standard therapies can create a synergistic effect. When combined with pharmacological treatments or psychotherapy, they may enhance efficacy while minimizing side effects associated with medications alone.
It’s crucial for healthcare providers to evaluate each patient’s unique needs when considering nutritional strategies. A tailored approach ensures that individuals receive optimal benefits from both their dietary interventions and conventional therapeutic methods.
Physical Therapies and Medication: A Holistic Treatment Plan
Physical therapies play a crucial role in the comprehensive management of catatonia. When combined with medication, they provide a holistic approach that addresses both physical and psychological aspects of the condition. Techniques such as physiotherapy can help mitigate muscle stiffness and enhance mobility, which are common challenges faced by individuals with catatonia.
Incorporating movement-based therapies encourages engagement with the body and fosters greater awareness of physical sensations. This is particularly beneficial for patients who may be experiencing psychomotor agitation or immobility. Additionally, regular physical activity can contribute to improved mood and overall well-being.
Medication remains essential in managing underlying symptoms associated with catatonia. However, its effectiveness can be amplified when paired with targeted exercise regimens or occupational therapy sessions focused on daily living skills. These interventions work synergistically to improve quality of life.
By adopting this multifaceted strategy, healthcare providers can better support patients through their recovery journey. A combination of medication and physical therapies creates a pathway towards healing that respects individual needs while promoting active participation in treatment.
Neuromodulation Techniques in Combination with Pharmacotherapy
Neuromodulation techniques are gaining traction as adjunct therapies in treating catatonia. These methods aim to alter neural activity, offering hope for patients who do not respond well to traditional pharmacotherapy alone. Techniques such as transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT) have shown promise.
When combined with pharmacological treatments, neuromodulation can enhance overall efficacy. For example, TMS may increase the effectiveness of antidepressants by stimulating specific brain regions associated with mood regulation. This synergistic approach caters to various underlying neurobiological mechanisms in catatonia.
Additionally, ECT has been a longstanding treatment option that works exceptionally well when paired with medications like benzodiazepines or antipsychotics. The combination can reduce symptoms more rapidly than either method alone, providing quicker relief for patients in distress.
Furthermore, these techniques offer the potential to minimize medication dosages and their side effects. By integrating neuromodulation into treatment plans, clinicians can create a more comprehensive strategy tailored to individual patient needs.
Tailoring Combination Therapies to Individual Patient Needs
Tailoring combination therapies in catatonia is essential for optimizing treatment outcomes. Each patient presents unique symptoms and underlying conditions that require a personalized approach. A thorough assessment of the individual’s medical history, current medications, and specific manifestations of catatonia can guide clinicians in selecting the most effective therapeutic combinations.
Collaboration between healthcare providers is key. Psychiatrists, neurologists, and psychologists must work together to develop a holistic plan that addresses both biological and psychological aspects of catatonia. Monitoring responses to treatment facilitates adjustments based on efficacy and tolerability.
Patient engagement plays a crucial role as well. Educating patients about their condition empowers them to participate actively in their treatment decisions. This collaboration fosters trust between patients and providers, leading to better adherence to treatment plans.
Regular follow-ups are necessary for ongoing evaluation of therapy effectiveness. Changes in symptoms or side effects may prompt modifications in medication dosages or the introduction of additional therapies tailored specifically for each patient’s evolving needs.
Monitoring and Managing Interactions in Combination Treatments
The complexity of combination therapies in catatonia necessitates careful monitoring and management of interactions between various treatments. Each therapy, whether pharmacological or non-pharmacological, can influence the efficacy and safety profiles of the others. Clinicians must be vigilant when integrating multiple modalities to ensure that potential adverse effects are minimized while therapeutic benefits are maximized.
Regular assessments should be conducted to monitor patient responses to these combinations. This includes tracking symptom relief as well as any emerging side effects. Adjustments may be required based on individual tolerances and reactions.
Collaboration among multidisciplinary teams is crucial for optimizing treatment plans tailored to each patient’s unique needs. Open lines of communication between healthcare providers can facilitate timely interventions if complications arise. By prioritizing patient safety through meticulous monitoring, clinicians can enhance the effectiveness of combination therapies in managing catatonia, ultimately leading to improved outcomes for those affected by this complex condition.