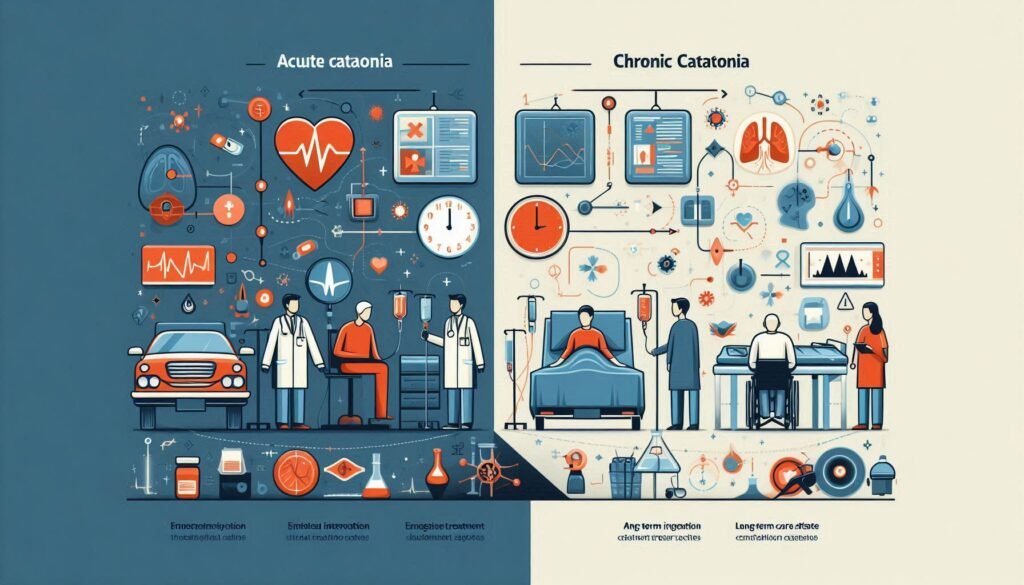
Catatonia, a complex neuropsychiatric condition, presents in two distinct forms: acute and chronic. Each variant requires tailored treatment approaches that can significantly impact the lives of those affected. Understanding how to manage acute versus chronic catatonia is essential for healthcare professionals, caregivers, and families alike.
In this blog post, we will delve into the nuances of distinguishing between these two forms of catatonia. We’ll explore effective strategies for managing each type, from immediate interventions to long-term care plans. With insights on pharmacological and non-pharmacological treatments as well as rehabilitation strategies, you’ll gain a comprehensive understanding of this often-misunderstood condition.
Whether you’re seeking information for personal knowledge or professional practice, navigating the complexities of catatonia management can make all the difference in improving quality of life for individuals facing these challenges. Let’s embark on this journey together to uncover effective solutions tailored specifically to acute and chronic cases.
Distinguishing Acute from Chronic Catatonia: Key Diagnostic Criteria
Acute catatonia typically develops rapidly, often within hours or days. It is characterized by a marked change in motor behavior, including immobility, rigidity, and peculiar postures. Diagnosis relies heavily on clinical observation of these symptoms alongside psychiatric assessments.
In contrast, chronic catatonia persists for an extended period—usually weeks to months. Patients may exhibit similar motor features but often demonstrate more subtle signs that can fluctuate over time. This form can be associated with underlying mental disorders like schizophrenia or mood disorders.
Key diagnostic criteria also include the duration of symptoms and their impact on daily functioning. Acute cases demand immediate attention due to their sudden onset and potential for severe distress. Chronic situations require careful evaluation of personal history and previous episodes.
Clinicians utilize standardized assessment tools such as the Bush-Francis Catatonia Rating Scale to aid in diagnosis. Understanding these distinctions is critical for developing effective treatment strategies tailored to each type’s unique challenges.
Acute Catatonia Management: Rapid Intervention Strategies
Acute catatonia requires immediate attention. Rapid intervention can significantly improve outcomes. Recognizing the symptoms early is crucial for effective management. Common signs include immobility, mutism, and abnormal posturing.
Benzodiazepines are often the first-line treatment in acute cases. They help relax muscle tension and reduce agitation quickly. Dosing should be tailored to the individual’s needs, ensuring both safety and effectiveness.
Electroconvulsive therapy (ECT) serves as a powerful option when benzodiazepines fail or if there’s severe distress. ECT can lead to rapid resolution of symptoms while minimizing potential complications associated with prolonged catatonia.
Monitoring vital signs during this phase is essential for patient safety. Close observation allows healthcare providers to adjust treatments promptly based on response levels and any emerging side effects from medications used in managing acute episodes.
Chronic Catatonia: Long-Term Treatment Plans and Considerations
Chronic catatonia presents unique challenges that necessitate comprehensive long-term treatment plans. These strategies often incorporate a multi-disciplinary approach, ensuring collaboration between psychiatrists, psychologists, and occupational therapists. This diverse team can provide tailored interventions based on the individual’s specific needs.
Long-term management typically includes ongoing psychotherapy to address underlying psychological issues and build coping mechanisms. Cognitive-behavioral therapy (CBT) is particularly beneficial for promoting engagement and reducing anxiety associated with symptoms.
Pharmacological options should also be reassessed regularly. Medications like benzodiazepines or atypical antipsychotics may need adjustments over time to optimize efficacy while minimizing side effects in chronic cases.
Regular monitoring of both mental health status and physical well-being is crucial. Ensuring patients have access to support services further enhances their quality of life, providing essential resources for social integration and daily functioning within their communities.
Pharmacological Approaches: Differences in Acute and Chronic Cases
Pharmacological approaches to managing catatonia differ significantly between acute and chronic cases. In acute situations, rapid intervention is crucial. Benzodiazepines are often the first line of treatment due to their sedative effects and ability to alleviate symptoms quickly. Dosing adjustments may be necessary, but immediate relief is typically the goal.
On the other hand, chronic catatonia requires a more nuanced approach. Antipsychotic medications can play a significant role in long-term management. These medications help stabilize mood and reduce psychotic features that might contribute to ongoing catatonic states.
Consideration of side effects also varies with duration of illness. Acute treatments focus on quick symptom control, while chronic care must balance efficacy with minimizing adverse reactions over time.
Moreover, combining pharmacotherapy with psychotherapy enhances outcomes in both scenarios but requires tailored strategies based on individual patient needs and histories.
Non-Pharmacological Interventions: Adapting Techniques for Duration
Non-pharmacological interventions play a significant role in managing both acute and chronic catatonia. These approaches can be tailored based on the duration of the condition, focusing on enhancing engagement and reducing symptoms.
For acute cases, immediate strategies include sensory stimulation techniques such as music therapy or art activities. These methods help to draw individuals out of their withdrawal state quickly. They capitalize on brief interactions that can spark interest and improve responsiveness.
In contrast, long-term management for chronic catatonia requires more structured interventions. Cognitive-behavioral therapies (CBT) are effective in addressing underlying thoughts and behaviors contributing to persistent symptoms. This approach fosters gradual change over time.
Mindfulness practices also show promise for chronic patients. Techniques like meditation or yoga encourage relaxation while promoting self-awareness, which can facilitate emotional processing that may have been stifled during episodes of catatonia.
Neuroplasticity in Chronic Catatonia: Implications for Treatment
Neuroplasticity refers to the brain’s ability to reorganize itself by forming new neural connections. In chronic catatonia, this phenomenon plays a crucial role in treatment strategies. As patients experience prolonged symptoms, their brains may adapt by rewiring pathways related to motor control and emotional regulation.
Harnessing neuroplasticity can lead to significant improvements for those suffering from chronic catatonia. Therapeutic interventions that promote this reorganization can provide hope for recovery. Techniques such as cognitive-behavioral therapy (CBT) or specialized physical rehabilitation exercises help stimulate brain areas affected by catatonia.
Additionally, incorporating mindfulness practices and meditation into treatment plans has been shown to enhance neuroplastic changes. These approaches foster an environment where patients can learn new coping mechanisms and regain lost functions over time.
Understanding the implications of neuroplasticity allows clinicians to tailor treatments effectively. By focusing on enhancing these brain adaptations, healthcare providers can offer more personalized care that addresses individual patient needs in managing chronic catatonia.
Preventing Acute Catatonia from Becoming Chronic: Early Intervention
Preventing acute catatonia from becoming chronic relies heavily on early intervention and prompt recognition of symptoms. Timely assessment is crucial. Healthcare providers must be vigilant in identifying the initial signs, such as immobility or unusual posturing, to initiate immediate treatment.
Early diagnosis often involves a thorough clinical evaluation and ruling out underlying medical conditions. This approach allows for targeted interventions that can effectively address the root causes of acute catatonia before it escalates.
Implementing supportive care measures during this phase is equally important. Supportive environments reduce stressors that may exacerbate symptoms, promoting recovery through stability and reassurance.
Engaging caregivers and family members in education about the condition fosters better understanding and support systems at home. Empowered families can help monitor changes in behavior, ensuring swift action if symptoms reappear or worsen.
Quality of Life Considerations in Chronic Catatonia Management
Quality of life is a crucial aspect when managing chronic catatonia. Patients often experience significant impairments in daily functioning, emotional well-being, and social interactions. Addressing these areas can greatly enhance their overall quality of life.
Social support plays an essential role for individuals with chronic catatonia. Encouraging family involvement and community connections fosters a sense of belonging and reduces feelings of isolation. Engaging with peer support groups can also provide valuable insights and shared experiences that help patients feel understood.
Therapeutic interventions are vital in improving the quality of life for those affected by chronic catatonia. Cognitive-behavioral therapy (CBT) or art therapy may assist patients in expressing their emotions while developing coping strategies to manage symptoms more effectively.
Additionally, regular assessments should be conducted to monitor changes in health status, environmental factors, and personal goals. This ongoing evaluation helps tailor treatment plans specifically to meet the evolving needs of each patient, enhancing their ability to navigate daily challenges successfully.
Monitoring and Adjusting Treatment: Acute vs. Chronic Protocols
Monitoring treatment in acute catatonia is crucial due to its dynamic nature. Symptoms can escalate rapidly, necessitating frequent assessments. Healthcare providers often implement daily evaluations to gauge responses to interventions. This allows for timely adjustments, ensuring effective management.
In contrast, chronic catatonia requires a different approach. Patients may stabilize over time but still need regular check-ins. Monitoring focuses on long-term efficacy and side effects of treatments rather than immediate changes in condition. Adjustments might be less frequent but are essential for maintaining quality care.
Both protocols involve collaborative efforts among healthcare professionals, caregivers, and patients themselves. Open communication fosters an environment where concerns can be addressed promptly and efficiently.
Data collection plays a key role as well; tracking symptoms through standardized scales helps identify patterns that inform treatment modifications. Keeping meticulous records ensures that both acute episodes and chronic conditions receive the attention they require while maximizing patient outcomes.
Rehabilitation Strategies: Tailoring Approaches to Catatonia Duration
Rehabilitation strategies for catatonia must be carefully tailored based on whether the condition is acute or chronic. For acute cases, swift intervention is crucial. This often involves immediate medical attention and intensive support to stabilize the patient. Techniques like structured environments can help patients regain functionality.
For those with chronic catatonia, rehabilitation takes a different approach. It focuses on gradual reintegration into daily life while addressing underlying issues that contribute to the prolonged state. Therapies may include cognitive-behavioral techniques and social skills training aimed at enhancing engagement with the environment.
Both approaches should prioritize individual needs and incorporate family involvement whenever possible. Regular assessments ensure that treatment evolves alongside changes in each patient’s condition, ultimately aiming for improved quality of life and better coping mechanisms long-term.
Effective management of both acute and chronic catatonia requires an understanding of these nuances in rehabilitation strategy, promoting a path towards recovery that respects each individual’s experience.


