Diagnosing catatonia in patients with Autism Spectrum Disorder (ASD) presents a unique challenge for clinicians. The overlapping symptoms of both conditions can lead to confusion and misdiagnosis, making it crucial for healthcare providers to differentiate between them accurately.
As awareness grows around the complexities of autism-related catatonia, understanding how to navigate this nuanced diagnostic landscape becomes essential. By delving into specific symptoms, behaviors, and assessment strategies, we can better equip ourselves to identify catatonia in autistic individuals effectively.
This blog post will guide you through the key aspects of diagnosing catatonia within the context of autism, ensuring that those affected receive appropriate care tailored to their needs.
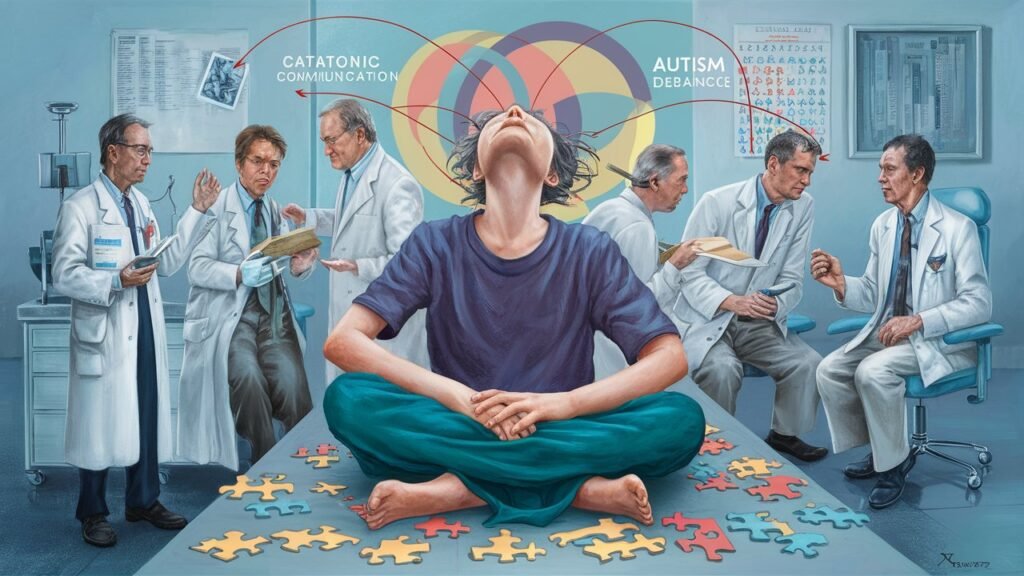
Understanding the Overlap: Catatonia and Autism Spectrum Disorders
The intersection of catatonia and Autism Spectrum Disorder (ASD) is an area that requires careful examination. Both conditions share a range of symptoms that can complicate diagnosis, making it essential to understand their similarities and differences. For instance, individuals with ASD may exhibit rigid behaviors or unusual responses to stimuli, which can mimic catatonic features.
Catatonia itself includes a spectrum of motor disturbances such as immobility, mutism, and posturing. These symptoms might overlap with the non-verbal communication challenges often seen in autistic individuals. This overlap can lead to misinterpretation during clinical assessments.
Moreover, stressors like sensory overload or changes in routine may exacerbate both autism-related behaviors and catatonic symptoms. Differentiating between these reactions demands an informed perspective on how each condition manifests in various contexts.
Awareness of this interplay not only enhances diagnostic accuracy but also informs treatment approaches tailored specifically for patients navigating both challenges. Understanding this complexity is vital for effective intervention strategies.
Recognizing Catatonic Symptoms in the Context of Autistic Behaviors
Recognizing catatonic symptoms in individuals with autism can be challenging due to the similarities between both conditions. Autistic behaviors, such as repetitive movements and rigid routines, may mask or mimic signs of catatonia. Observers must remain vigilant to differentiate these nuances effectively.
Key catatonic features include motor immobility, excessive purposeless movement, and peculiar posturing. These symptoms often present suddenly and can vary significantly from a person’s baseline behavior. Being aware of sudden shifts is crucial for accurate recognition.
Another important aspect is assessing changes in responsiveness. While many autistic individuals may exhibit limited social engagement, catatonia frequently involves marked withdrawal or unresponsiveness that differs from typical autistic traits.
Consider emotional responses too. An individual experiencing catatonia might show a sudden lack of affect or an inability to engage emotionally—contrasting sharply with their usual expressions related to joy or frustration within the autism spectrum context.
Differential Diagnosis: Distinguishing Catatonia from Autism Exacerbation
Differentiating catatonia from an exacerbation of autism can be complex. Both conditions manifest with overlapping symptoms, making accurate diagnosis crucial for effective treatment. Clinicians must carefully evaluate the patient’s behavioral patterns to identify key distinctions.
Catatonia may present as marked immobility, mutism, or echolalia. In contrast, autistic exacerbation typically involves heightened anxiety, irritability, or repetitive behaviors. Recognizing these differences is vital in guiding appropriate interventions and support strategies.
Another critical factor is the duration and context of symptoms. Catatonic states often develop suddenly and may fluctuate throughout the day. Autistic behaviors tend to be more consistent over time but can worsen during periods of stress or change in routine.
Effective communication with caregivers also plays a significant role in this differential diagnosis process. Gathering detailed accounts about a patient’s behavior during both calm and stressful situations can yield insights that clarify whether they are experiencing catatonia or simply an intensification of their autism-related traits.
Adapting Diagnostic Criteria for Catatonia in Autistic Individuals
Adapting diagnostic criteria for catatonia in autistic individuals is essential given the unique characteristics of autism spectrum disorder (ASD). Traditional definitions of catatonia may not fully capture the nuances seen in patients with ASD. Therefore, clinicians must consider how behavioral expressions differ among these populations.
For instance, repetitive movements or echolalia might be misinterpreted as catatonic symptoms. A thorough understanding of baseline behaviors allows healthcare professionals to identify genuine episodes of catatonia more accurately. This requires careful observation and contextual analysis.
Incorporating input from caregivers can also enhance the diagnostic process. They often have insights into changes in behavior that may indicate a shift toward catatonia. Tailoring assessments involves both qualitative and quantitative measures to ensure reliability.
Moreover, modifications should include consideration for sensory sensitivities common within autistic individuals. These adaptations support a comprehensive evaluation while reducing potential misdiagnosis, leading to better management strategies tailored specifically for this population’s needs.
The Role of Behavioral Observation in Autism-Related Catatonia
Behavioral observation is vital in assessing catatonia among individuals with autism spectrum disorder (ASD). It allows caregivers and clinicians to gather essential data on a patient’s behavior over time. Observing patterns of movement, communication, and social interaction can reveal critical insights.
In many cases, autistic behaviors might mask or mimic the signs of catatonia. For instance, echolalia or repetitive movements may be confused with catatonic rigidity or stupor. Careful observation helps differentiate these behaviors from true catatonic symptoms.
The context in which behaviors occur also plays a crucial role. Engaging with patients during various activities can help identify moments when unusual behavior surfaces. Notably, changes in environment or routine could trigger an escalation of symptoms.
Documentation of observed behaviors assists healthcare professionals in making informed decisions about diagnosis and treatment approaches. This ongoing assessment contributes significantly to understanding the nuances between autism-related traits and potential catatonia manifestations.
Communication Challenges: Assessing Non-Verbal Autistic Patients for Catatonia
Assessing non-verbal autistic patients for catatonia presents unique communication challenges. These individuals may struggle to express their feelings or discomfort verbally, making identification of symptoms complex. Therefore, caregivers and clinicians must rely heavily on alternative forms of communication.
Observing body language is essential in these assessments. Subtle shifts in posture or eye contact can provide critical insights into a patient’s emotional state. For instance, withdrawal from interaction might signal distress rather than mere preference for solitude.
In addition to physical cues, environmental factors play a significant role in understanding a non-verbal patient’s condition. Changes in surroundings can trigger anxiety or sensory overload, potentially mimicking catatonic symptoms. Awareness of such triggers aids accurate interpretation of behaviors.
Utilizing visual supports like picture exchange systems can enhance assessment efforts as well. Charts and symbols offer alternative pathways for expression, allowing patients to communicate needs more effectively while facilitating a better evaluation process for potential catatonia.
Sensory Processing Considerations in Autism-Catatonia Assessment
Sensory processing can significantly influence the presentation of catatonia in individuals with autism spectrum disorder. Many autistic patients experience heightened or diminished responses to sensory input, which may complicate their behavioral expressions. Understanding these variations is crucial for accurate assessment.
When assessing a patient for catatonia, clinicians should consider how sensory overload or deprivation might manifest as withdrawal or immobility. For instance, an individual overwhelmed by stimuli may appear catatonic due to an inability to engage rather than true motor dysfunction.
Additionally, some patients might display repetitive movements or other behaviors often mistaken for catatonia but are rooted in sensory-seeking actions. This blends the lines between typical autistic behavior and potential catatonic symptoms.
Assessing environmental factors that contribute to sensory experiences can offer insights into the patient’s condition. Tailoring assessments with sensitivity toward sensory issues leads to more accurate observations and better diagnosis outcomes.
Collaborative Diagnosis: Integrating Autism and Catatonia Expertise
Diagnosing catatonia in patients with autism spectrum disorder requires a multidisciplinary approach. Autism specialists, psychiatrists, and neurologists must collaborate to ensure an accurate diagnosis. Each professional brings unique insights that contribute to understanding the complexities of both conditions.
Effective communication among team members is essential for sharing observations and experiences. This collaboration can help identify overlapping symptoms while clarifying distinct features of catatonia. Regular meetings allow for comprehensive discussions about patient cases, leading to more nuanced assessments.
Family involvement also plays a crucial role in this collaborative effort. Caregivers can provide valuable context regarding changes in behavior or mood that may indicate emerging catatonic symptoms. Their firsthand experience helps professionals weigh information against typical autistic traits.
Integrating expertise across disciplines enriches diagnostic accuracy and fosters tailored treatment plans. Such collaboration leads to better outcomes for individuals facing this dual challenge by ensuring they receive the most appropriate care based on their specific needs.
Longitudinal Monitoring: Tracking Catatonic Symptoms in Autistic Patients
Longitudinal monitoring is essential in understanding catatonia within the autism spectrum. Tracking symptoms over time allows healthcare professionals to identify patterns and fluctuations in behavior. This approach provides valuable insights into how catatonic features may evolve or worsen.
Regular assessments help differentiate between typical autistic behaviors and those indicative of catatonia. By maintaining consistent observations, caregivers can document changes that might otherwise go unnoticed during sporadic visits. This data becomes crucial for developing personalized treatment plans tailored to individual needs.
Engaging with families also plays a pivotal role in longitudinal monitoring. Caregivers often witness subtle shifts in behavior at home, which can inform clinical evaluations. Their insights are integral to creating a comprehensive picture of the patient’s condition.
Utilizing standardized measurement tools alongside observational reports enhances accuracy in tracking symptoms. These combined efforts contribute significantly to effective diagnosis and intervention strategies, ensuring individuals receive appropriate care as their conditions change over time.
Treatment Implications of Accurate Diagnosis in Autism-Related Catatonia
Accurate diagnosis of catatonia in patients with Autism Spectrum Disorder is crucial for effective treatment planning. Understanding the distinct presentation of catatonic symptoms within this population can lead to more tailored therapeutic approaches.
When catatonia is identified, treatment strategies may differ significantly from those typically employed for autism alone. Psychopharmacological interventions, such as benzodiazepines or atypical antipsychotics, have shown effectiveness in alleviating catatonic features. Additionally, integrating supportive therapies like occupational therapy or behavioral interventions can enhance overall functioning.
Families and caregivers play a vital role in the management process. Providing education about recognizing signs and understanding how these symptoms interact with autistic behaviors will empower them to advocate effectively for their loved ones.
Regular follow-ups are essential to monitor responses to treatment and make necessary adjustments as needed. This collaborative approach ensures that individuals receive comprehensive care addressing both their autism and any emergent catatonic symptoms.
A nuanced understanding of how to diagnose catatonia in patients with Autism Spectrum Disorder not only aids clinicians but also enhances the quality of life for those affected by these complex conditions.