Understanding catatonia is crucial, especially as awareness about mental health continues to grow. The evolution of catatonic symptoms over time can be perplexing for both individuals experiencing them and their loved ones. Catatonia isn’t a singular experience; it presents a range of symptoms that can shift dramatically throughout its course.
From the initial signs to potential long-term effects, recognizing these changes is vital for effective management and support. In this blog post, we will explore the different phases of catatonia, how symptoms manifest and fluctuate, and what influences their trajectory over time. Whether you are seeking insight for yourself or someone you care about, this comprehensive examination aims to shed light on an often-misunderstood condition while providing valuable information on monitoring progress and seeking appropriate interventions. Join us as we delve into the intricate journey of catatonic symptoms through various stages and experiences!
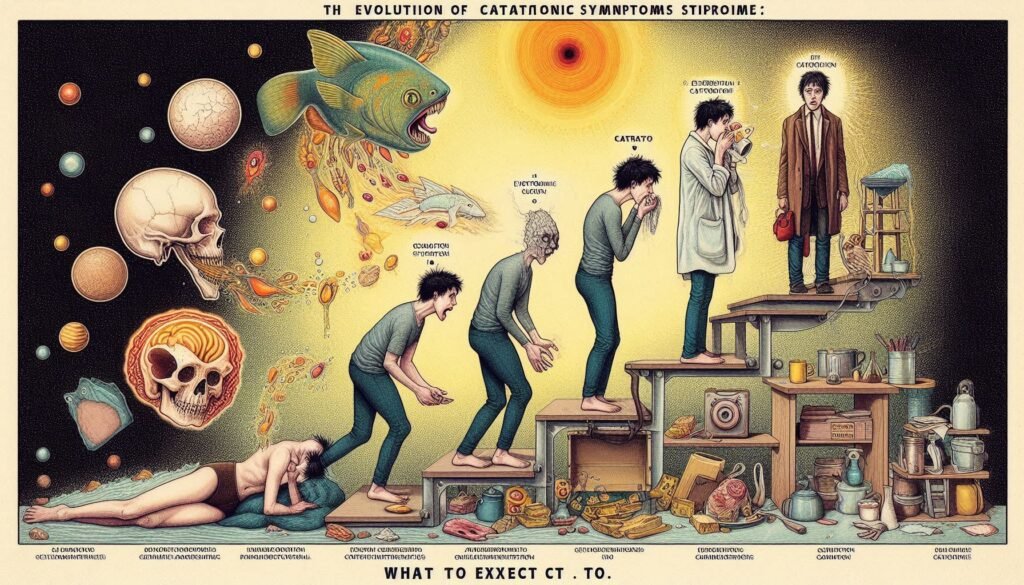
The Onset of Catatonia: Early Signs and Symptoms
The onset of catatonia can be subtle, often mistaken for stress or other mental health issues. Early signs typically include a noticeable decrease in responsiveness and engagement with the environment. Individuals may appear withdrawn, exhibiting reduced eye contact and lack of verbal communication.
Physical manifestations can also emerge during this phase. Some people may adopt unusual postures or exhibit limited movement, which might go unnoticed at first. A person could remain still for extended periods or display motor abnormalities like stiff limbs.
Moreover, behavioral changes such as agitation or unpredictable emotional responses may surface early on. These fluctuations can confuse family members who are trying to understand what is happening.
Recognizing these symptoms promptly is essential for timely intervention. Awareness of these initial signs can help individuals seek appropriate support and treatment before more severe symptoms develop, paving the way for better management outcomes in the future.
Acute Phase of Catatonia: Characteristic Symptom Patterns
During the acute phase of catatonia, symptoms become more pronounced and can significantly impact an individual’s functionality. One primary characteristic is marked psychomotor agitation or retardation. This means a person may exhibit excessive movement or appear completely immobile.
Another common symptom during this phase is waxy flexibility. Here, individuals may maintain positions into which they are placed for extended periods, resembling a doll-like rigidity. This peculiarity can often be startling to observers who are unfamiliar with these behaviors.
Echolalia and echopraxia also emerge prominently in this stage. Individuals might involuntarily mimic speech or movements made by others, showcasing their struggle to communicate authentically while caught in the grip of catatonic states.
Additionally, emotional responses may fluctuate dramatically during this time. Some individuals might display extreme emotional lability—shifting from laughter to tears within moments—further complicating diagnosis and treatment efforts as these patterns evolve rapidly.
Fluctuations in Catatonic Symptoms: Understanding Variability
Catatonic symptoms are not static; they often fluctuate, creating variability in how individuals experience this condition. These fluctuations can be attributed to various factors including stressors, changes in environment, or underlying medical issues. Some patients may exhibit sudden episodes of immobility one day and increased agitation the next.
Understanding these variations is crucial for caregivers and healthcare providers. For some individuals, symptoms might intensify during times of emotional distress or physical illness. Conversely, periods of calmness could lead to temporary remission of symptoms.
This inconsistency complicates diagnosis and treatment strategies. It requires careful observation to track symptom patterns over time. Recognizing that catatonia can manifest differently from day to day helps tailor effective interventions.
Furthermore, awareness of fluctuating symptoms fosters empathy among friends and family members who may struggle to comprehend the unpredictable nature of catatonia. Each individual’s journey highlights a unique set of challenges that warrant understanding and support.
Chronic Catatonia: Long-term Symptom Manifestations
Chronic catatonia can present a complex array of long-term symptoms that significantly impact an individual’s daily life. Unlike the acute phase, which may resolve with treatment, chronic manifestations often persist and evolve over time. Patients might experience enduring motor disturbances such as rigidity or posturing, making movement challenging.
Emotional symptoms can also linger. Individuals may exhibit profound apathy or emotional blunting, leading to difficulties in social interactions and relationships. This disconnection often exacerbates feelings of isolation and depression.
Cognitive aspects should not be overlooked either; some patients report memory issues or difficulty concentrating. These cognitive challenges can interfere with daily tasks and responsibilities, affecting overall quality of life.
Understanding these long-lasting symptoms is crucial for caregivers and healthcare providers alike. Tailoring support strategies becomes essential for improving patient outcomes while addressing their unique needs over time.
Factors Influencing the Course of Catatonic Symptoms
Catatonic symptoms can vary significantly from one individual to another. Several factors influence their course, including underlying mental health conditions. Disorders such as schizophrenia, mood disorders, and autism spectrum disorders often present catatonia in diverse ways.
Biological aspects play a vital role too. Genetic predispositions can make some individuals more susceptible to experiencing catatonia during stressful events or episodes of psychosis. Neurotransmitter imbalances are also crucial, particularly those involving dopamine and GABA.
Environmental triggers further complicate the picture. Stressful life events, trauma, or significant changes in routine can exacerbate symptoms. Support systems—like family and friends—can either buffer against these stressors or contribute to symptom escalation.
Treatment history impacts how symptoms unfold over time. Previous interventions may shape future responses to therapy or medication adjustments. Understanding these factors helps clinicians tailor treatment plans effectively for each patient’s unique journey with catatonia.
Treatment Response: How Symptoms Change with Intervention
Treatment for catatonia often leads to significant changes in symptoms. Early intervention is crucial, as it can drastically alter the course of the disorder. Patients may respond positively to medications such as benzodiazepines or atypical antipsychotics. These treatments aim to alleviate acute symptoms and restore normal functioning.
Psychotherapy also plays a vital role in managing catatonic symptoms. Cognitive-behavioral therapy (CBT) can help patients understand their experiences and develop coping mechanisms. Combining medication with therapy tends to yield better outcomes than either approach alone.
Electroconvulsive therapy (ECT) remains an effective option for severe cases that do not respond well to medications or psychotherapy. It may lead to rapid symptom resolution, especially when other interventions fail.
Monitoring response during treatment is essential; modifications may be necessary based on individual progress. Tracking these changes ensures that the most effective strategies are employed, ultimately improving quality of life for individuals affected by catatonia.
Residual Symptoms: Lingering Effects After Acute Episode
Residual symptoms can linger long after an acute episode of catatonia. These effects vary widely among individuals, impacting their daily lives and overall functioning. Patients may experience persistent motor abnormalities, such as stiffness or unusual postures that remain even when the immediate crisis has subsided.
Cognitive challenges are also common during this phase. Individuals might struggle with concentration, memory retention, or decision-making skills. Such difficulties can hinder social interactions and workplace performance, leading to frustration and isolation.
Emotional disturbances often follow a bout of catatonia as well. Anxiety and depression may surface in the wake of physical recovery, complicating the healing process further. It’s essential for those recovering to acknowledge these emotional changes and seek appropriate support.
Understanding residual symptoms is crucial for caregivers and healthcare providers. Awareness helps foster patience and compassion while guiding treatment plans tailored to each individual’s evolving needs throughout recovery.
Relapse and Recurrence: Recognizing Signs of Symptom Return
Relapse and recurrence of catatonic symptoms can be challenging for both individuals and their caregivers. Recognizing early signs is vital in managing these episodes effectively. Symptoms may re-emerge subtly, often resembling initial manifestations like decreased responsiveness or unusual postures.
People experiencing a relapse may show increased withdrawal from social interactions or changes in speech patterns. These behavioral shifts can sometimes be mistaken for stress or fatigue, making it crucial to maintain awareness of previous symptomatology.
Mood fluctuations might also signal a potential return of catatonia. Individuals could display heightened anxiety, irritability, or depression before the onset of more severe symptoms. Monitoring these emotional states provides valuable insights into one’s mental health trajectory.
Early intervention plays a significant role in mitigating the severity of relapses. If you notice any warning signs indicating a possible recurrence, seeking professional help promptly can make a substantial difference in outcomes and overall recovery journeys.
Recovery Trajectories: Variability in Symptom Resolution
Recovery from catatonia can take various paths, making it a unique experience for each individual. Some people may find their symptoms resolve quickly with timely intervention, while others might face a more prolonged journey. This variability is partly due to the underlying causes of catatonia and how they interact with an individual’s overall health.
Factors like age, mental health history, and the presence of co-occurring disorders play significant roles in recovery trajectories. For instance, younger patients or those without prior psychiatric issues often show quicker improvement than older individuals or those battling multiple conditions at once.
Additionally, social support systems can greatly influence outcomes. A strong network of family and friends may help facilitate faster recovery by providing emotional backing and assistance during challenging times.
Understanding these diverse trajectories is essential for both patients and caregivers. It helps set realistic expectations regarding treatment plans while emphasizing that progress isn’t always linear; setbacks are common but manageable components of the healing process.
Long-term Monitoring: Tracking Catatonic Symptoms Over Time
Long-term monitoring of catatonic symptoms is crucial for understanding their evolution and managing the condition effectively. Regular assessments can help identify changes in symptom patterns, allowing healthcare professionals to tailor interventions appropriately.
Tracking these symptoms over time offers insights into how individual experiences may differ. Some individuals may see a gradual reduction in severity, while others might face persistent challenges or relapses. Documenting these fluctuations not only informs treatment but also fosters open communication between patients and caregivers.
Moreover, long-term monitoring enables early detection of complications or new episodes of catatonia. This proactive approach ensures timely intervention when needed, improving overall outcomes for those affected.
Engaging with support networks during this process adds another layer of reassurance for both patients and families. Establishing coping mechanisms through education about catatonia empowers individuals to better navigate their journey.
By keeping a close eye on symptom progression and maintaining ongoing dialogue with mental health professionals, individuals experiencing catatonic symptoms can foster a more hopeful outlook on their future well-being.


