Cerebrovascular events can have profound effects on the brain, influencing not just physical health but also mental well-being. Among the lesser-discussed consequences of these incidents is catatonia, a complex neuropsychiatric condition that can arise in response to strokes or other vascular issues. The connection between cerebrovascular injuries and catatonic states is both intriguing and concerning.
Understanding how an ischemic stroke, hemorrhagic event, or even transient ischemic attacks (TIAs) can trigger such dramatic changes in behavior opens doors for better diagnosis and treatment options. As we delve into this topic, we’ll explore the mechanisms behind these occurrences, their symptoms, and ways to manage them effectively. Whether you are a healthcare professional seeking knowledge or someone interested in understanding this phenomenon more deeply, there’s much to uncover about cerebrovascular events as triggers for catatonia.
Understanding Cerebrovascular-Induced Catatonia
Cerebrovascular-induced catatonia is a rare but significant phenomenon that arises after cerebrovascular events. Catatonia itself is characterized by abnormal motor behavior, which can range from immobility to excessive agitation. The relationship between the brain’s vascular health and these symptoms warrants close examination.
When blood supply to areas of the brain is compromised due to strokes or other cerebrovascular incidents, neurological functions become disrupted. This disruption may interfere with various neurotransmitter systems involved in mood and motor control, potentially precipitating catatonic states.
The onset of catatonia post-stroke can vary widely among individuals. Factors such as age, pre-existing mental health conditions, and the severity of the stroke play crucial roles in determining susceptibility.
Recognizing this condition early can significantly impact treatment outcomes. Prompt intervention not only addresses immediate symptoms but also aids in improving long-term recovery for affected patients. Understanding how cerebrovascular events trigger these episodes enhances awareness within both medical communities and caregivers alike.
Ischemic Stroke and Its Link to Catatonic States
Ischemic stroke occurs when blood flow to the brain is obstructed, typically by a clot. This interruption can lead to various neurological deficits. Among these deficits, catatonic states have emerged as a significant concern in clinical settings.
Research indicates that ischemic strokes can trigger catatonia through disruption in specific brain regions responsible for movement and behavior regulation. When areas such as the basal ganglia or prefrontal cortex are affected, patients may exhibit symptoms like immobility or mutism.
The onset of catatonia following an ischemic event often complicates diagnosis and treatment. Healthcare providers must differentiate between post-stroke effects and underlying psychiatric conditions, which requires careful assessment.
Understanding this link is crucial for timely intervention. Early recognition of catatonic symptoms allows for appropriate management strategies to be implemented quickly, potentially improving outcomes for affected individuals. Prompt treatment can also facilitate better rehabilitation prospects down the line.
Hemorrhagic Stroke and Catatonic Presentations
Hemorrhagic stroke occurs when a blood vessel in the brain ruptures, causing bleeding into the surrounding tissues. This type of stroke can lead to significant neurological deficits and complications. Among these is catatonia, a condition characterized by abnormal motor behavior and unresponsiveness.
Patients experiencing hemorrhagic strokes may display various catatonic symptoms, such as mutism or stupor. The disruption in normal brain function often leads to altered consciousness levels, which can further complicate diagnosis and treatment. Understanding the underlying mechanisms is crucial for effective management.
The relationship between hemorrhagic events and catatonia involves complex neurobiological processes. Damage from intracranial bleeding affects areas responsible for movement regulation and emotional response, contributing to catatonic states.
Timely identification of these symptoms can be challenging but essential for patient care. Clinicians must remain vigilant as early intervention may improve outcomes significantly for those affected by both conditions.
Transient Ischemic Attacks (TIAs) and Catatonia Risk
Transient Ischemic Attacks (TIAs) are often termed “mini-strokes.” They occur when blood flow to the brain is temporarily disrupted, leading to symptoms that usually resolve within minutes or hours. Despite their transient nature, TIAs can have significant long-term effects on mental health.
Research indicates a noteworthy correlation between TIAs and catatonic states. Individuals who experience multiple TIAs may develop neurological changes that increase vulnerability to psychiatric disorders, including catatonia. The brief periods of ischemia can affect neuronal pathways responsible for mood regulation and motor function.
Patients may present with abnormal postures or unresponsiveness following a TIA episode. These symptoms can mimic those found in full-blown catatonia but might be overlooked due to their transient presentation. This complicates timely diagnosis and treatment.
Healthcare providers must remain vigilant when assessing patients with a history of TIAs. Recognizing potential signs of catatonia early could lead to more effective interventions and better patient outcomes in this vulnerable population.
Cerebral Small Vessel Disease and Catatonic Symptoms
Cerebral small vessel disease (CSVD) is a condition that affects the small arteries in the brain. It can lead to various neurological issues, including cognitive decline and movement disorders. One of the lesser-known complications associated with CSVD is catatonia, which manifests as extreme behavioral changes.
Patients with CSVD may experience symptoms such as stupor, mutism, or posturing. These presentations are often mistaken for other psychiatric conditions, complicating diagnosis and treatment. The vascular changes in smaller vessels can disrupt normal brain function significantly.
Research suggests that reduced blood flow caused by CSVD contributes to these catatonic states. Ischemia impacts regions of the brain responsible for mood regulation and motor control. As a result, affected individuals may show signs of withdrawal or unresponsiveness.
Early recognition is crucial for effective management. Understanding this link between cerebral small vessel disease and catatonic symptoms can pave the way for more tailored interventions aimed at improving patient outcomes.
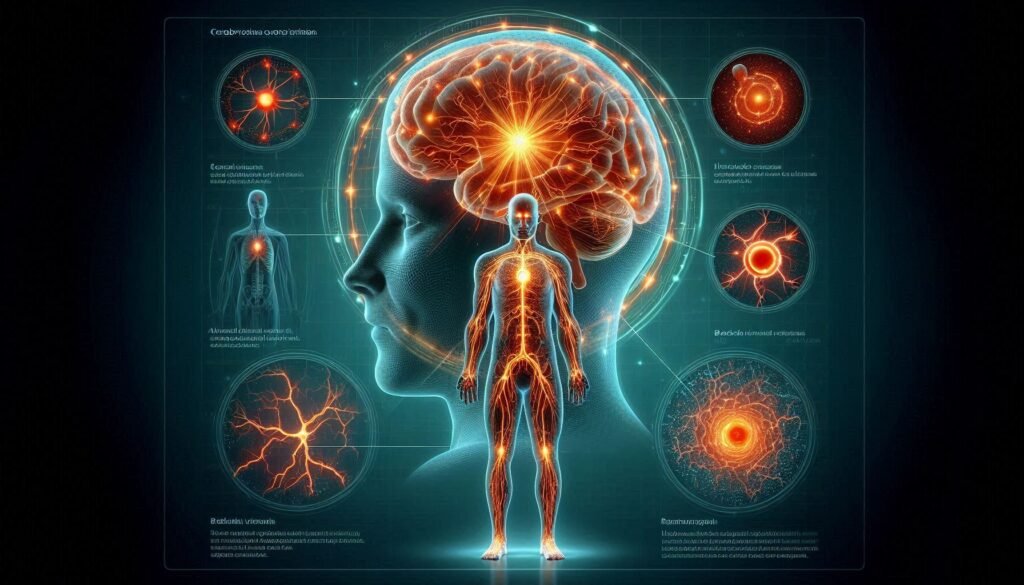
Neuroanatomical Correlates of Cerebrovascular Catatonia
Cerebrovascular events can lead to catatonia through various neuroanatomical pathways. Understanding these correlates is essential for diagnosing and treating affected individuals. The brain’s intricate network is vulnerable during strokes, potentially disrupting areas responsible for movement and behavior.
The basal ganglia play a significant role in motor control. Damage here can result in the characteristic immobility seen in catatonic states. Additionally, lesions affecting the frontal lobes may impair executive functioning and emotional regulation, further contributing to catatonia.
Another critical region is the thalamus, which acts as a relay station for sensory information. Disruption of its circuits can lead to altered consciousness or awareness, commonly observed in patients experiencing catatonic symptoms following cerebrovascular incidents.
Changes within white matter tracts due to small vessel disease might also influence connectivity between regions involved in mood and motor function. This complex interplay suggests that targeted interventions could benefit those suffering from this condition after cerebrovascular events.
Diagnostic Approaches for Post-Stroke Catatonia
Diagnosing post-stroke catatonia can be challenging due to overlapping symptoms with other neurological and psychiatric disorders. A thorough patient history is crucial, focusing on the timing of neurological events and any behavioral changes that followed. Gathering information from family members or caregivers adds valuable context.
Clinical assessments play a key role in diagnosis. Healthcare professionals often use standardized scales like the Bush-Francis Catatonia Rating Scale to identify specific catatonic features. This scale evaluates behaviors such as mutism, stupor, and rigidity.
Neuroimaging techniques also provide insight into underlying cerebrovascular issues. MRI scans may reveal infarcts or hemorrhages correlating with observed catatonic states, aiding in understanding the relationship between brain injury and symptom presentation.
Additionally, ruling out other conditions is essential for an accurate diagnosis. Blood tests, electroencephalograms (EEGs), and psychological evaluations help differentiate post-stroke catatonia from delirium or psychosis. Each step ensures a comprehensive approach to identifying this complex condition effectively.
Acute Management of Cerebrovascular-Induced Catatonia
Acute management of cerebrovascular-induced catatonia focuses on immediate assessment and intervention. Healthcare professionals prioritize ensuring the patient’s safety. This involves monitoring vital signs, addressing any underlying medical issues, and providing a supportive environment.
Pharmacological treatment is often initiated to alleviate catatonic symptoms. Benzodiazepines are commonly used due to their rapid onset in reducing anxiety and agitation. In some cases, atypical antipsychotics may also be considered for patients who do not respond adequately to benzodiazepines alone.
Non-pharmacological approaches can complement medication therapy. Engaging patients through gentle communication and structured activities can help reduce isolation and enhance responsiveness. Creating a calm atmosphere is essential for minimizing stressors that could exacerbate symptoms.
Collaboration among multidisciplinary teams ensures comprehensive care during this acute phase. Neurologists, psychiatrists, and rehabilitation specialists must work together to optimize recovery strategies tailored to each patient’s unique needs following their cerebrovascular event.
Long-Term Outcomes and Rehabilitation Strategies
Long-term outcomes for patients who experience cerebrovascular events that trigger catatonia can vary significantly. Many individuals may face persistent cognitive and emotional challenges, including difficulties with movement and communication. Understanding these potential repercussions is crucial for tailoring rehabilitation efforts.
Rehabilitation strategies should be multifaceted, combining physical, occupational, and speech therapies to address the broad spectrum of symptoms associated with catatonia. By focusing on improving mobility and functionality, therapists can help patients regain independence in daily activities.
Psychological support also plays a vital role in recovery. Cognitive-behavioral therapy (CBT) can assist in addressing anxiety or depression that often accompanies catatonic states following cerebrovascular incidents. Early intervention tends to yield better results.
Family involvement is essential throughout the rehabilitation process. Educating caregivers about the condition fosters a supportive environment conducive to healing. This collaborative approach enhances engagement from both patients and families, ultimately promoting better long-term outcomes post-cerebrovascular events.
Preventing Catatonia in Cerebrovascular Patients
Prevention is key when it comes to cerebrovascular events and the potential onset of catatonia. Patients who have experienced strokes or transient ischemic attacks (TIAs) should be monitored closely for early signs of neuropsychiatric symptoms. Early intervention can significantly reduce the risk.
Educating healthcare providers about the relationship between cerebrovascular conditions and psychiatric manifestations is essential. Regular assessments using standardized screening tools can help identify changes in behavior or mood that may precede catatonic states.
Moreover, implementing a multidisciplinary approach involving neurologists, psychiatrists, and rehabilitation specialists can enhance outcomes. Lifestyle modifications also play a crucial role; promoting physical activity, balanced nutrition, and controlling vascular risk factors like hypertension and diabetes are vital steps.
Incorporating cognitive therapies may bolster mental resilience against the psychological impacts following a stroke. Continuous education for both patients and families about recognizing warning signs empowers them to seek timely medical attention if behavioral changes occur.
By prioritizing prevention strategies tailored to individuals at high risk for cerebrovascular events as triggers for catatonia, we pave the way towards better management of these complex cases while improving overall quality of life.