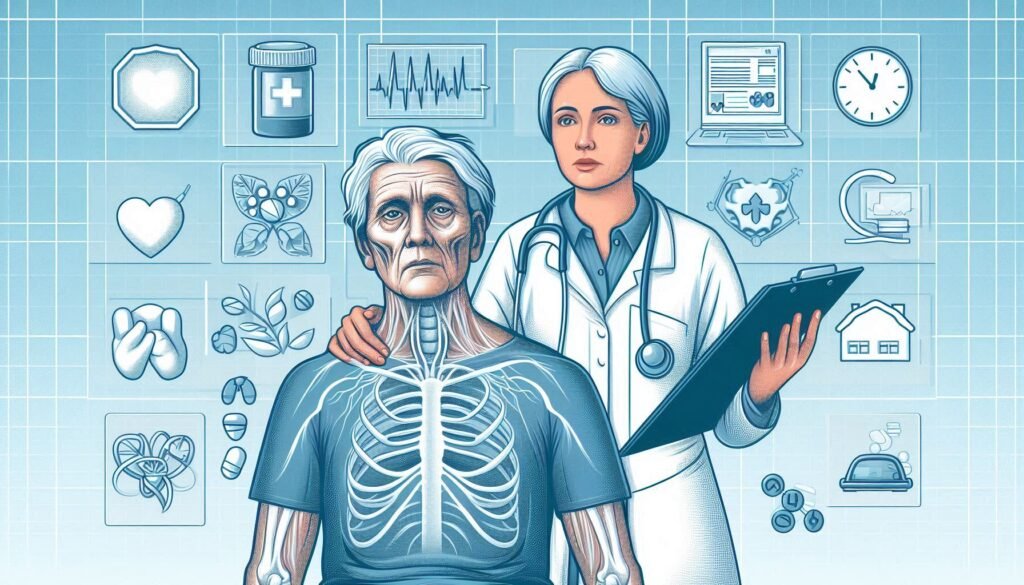
Catatonia is often shrouded in mystery, particularly when it appears in elderly patients. As we age, the presentation of psychiatric symptoms can become complex and challenging to navigate. For caregivers and healthcare professionals alike, recognizing catatonia’s unique characteristics within geriatric populations is crucial for proper diagnosis and treatment.
Diagnostic challenges in elderly patients with catatonic symptoms frequently stem from overlapping features with other conditions such as dementia or delirium. These silent struggles can significantly impact quality of life if left unrecognized or misdiagnosed. Understanding the nuances of these cases is essential for effective intervention.
This article will explore various aspects of diagnosing catatonia in older adults, providing insights into how to differentiate it from similar disorders, identify medication-induced causes, assess comorbidities, and utilize comprehensive evaluations to improve outcomes. Join us as we delve into the complexities surrounding this often-misunderstood condition affecting our aging population.
The Unique Presentation of Catatonia in Geriatric Populations
Catatonia manifests differently in elderly patients compared to younger individuals. While the classic symptoms include stupor, mutism, and posturing, older adults may present with atypical features. These can often resemble other psychiatric or neurological disorders, complicating diagnosis.
Elderly patients might exhibit increased withdrawal tendencies or changes in social engagement rather than overt catatonic behaviors. This subtlety can lead caregivers to overlook critical signs of catatonia. They might attribute these changes to age-related cognitive decline instead.
Additionally, physical ailments common in older populations can overshadow psychological symptoms. Factors such as chronic pain or mobility issues may contribute to a lack of movement and communication that mimics catatonia but arises from different causes.
Recognizing these unique presentations is essential for timely intervention. Misidentification risks prolonged suffering and inadequate treatment options for those affected by this debilitating condition. Understanding geriatric nuances allows healthcare providers to approach diagnosis more effectively.
Differentiating Catatonia from Dementia and Delirium in Older Adults
Differentiating catatonia from dementia and delirium in older adults is crucial for effective treatment. While all three conditions can present with altered mental status, their underlying mechanisms and symptoms vary significantly. Catatonia often manifests as motor disturbances, including immobility or excessive movement. This can be confused with the cognitive decline seen in dementia.
Dementia typically involves gradual memory loss and impaired reasoning skills, which may lead to misinterpretation of a catatonic state as simply confusion or apathy. Delirium, on the other hand, is characterized by acute onset fluctuations in attention and awareness. Unlike catatonia, delirium tends to arise suddenly due to medical issues like infections or metabolic imbalances.
A thorough assessment of history and symptom duration helps distinguish these disorders. Healthcare providers must consider behavioral patterns alongside cognitive assessments to avoid misdiagnosis that could hinder appropriate care for elderly patients experiencing catatonic symptoms.
Medication-Induced Catatonia: A Common Pitfall in Elderly Diagnosis
Medication-induced catatonia is a significant challenge in diagnosing elderly patients. Older adults often take multiple medications, increasing the risk of adverse reactions. These interactions can lead to symptoms that mimic primary psychiatric disorders, complicating accurate diagnosis.
Common culprits include antipsychotics and sedatives. The elderly may experience heightened sensitivity to these drugs due to age-related metabolic changes. This sensitivity can trigger catatonic features such as immobility or stupor, which may be misinterpreted by healthcare providers.
Moreover, the presentation of medication-induced catatonia can overlap with other conditions like dementia or delirium. Distinguishing between these requires careful history-taking and observation over time.
It is essential for clinicians to consider recent medication changes when assessing catatonic symptoms in older patients. A thorough drug review might reveal hidden causes that could steer treatment toward appropriate interventions rather than unnecessary psychiatric evaluations.
Comorbid Medical Conditions: Unmasking Hidden Causes of Late-Life Catatonia
Catatonia in elderly patients can often be overshadowed by existing medical conditions. These comorbidities complicate the diagnostic landscape, masking catatonic symptoms within a broader clinical picture. Conditions such as Parkinson’s disease, stroke, and dementia frequently coexist with catatonia, making identification challenging.
The interplay between these disorders can lead to misdiagnosis or delayed treatment. For instance, rigidity associated with Parkinson’s may mimic catatonic features. Similarly, cognitive decline seen in dementia may obscure underlying catatonic states that require attention.
Additionally, metabolic disturbances like electrolyte imbalances or infections can precipitate or exacerbate catatonia. Healthcare providers must remain vigilant when evaluating older adults with complex health profiles to avoid overlooking these critical connections.
Thorough assessments are essential for unmasking hidden causes of late-life catatonia. This includes comprehensive evaluations that consider all potential medical factors contributing to the patient’s presentation rather than relying solely on visible symptoms alone.
Neuroimaging in Geriatric Catatonia: Interpreting Age-Related Brain Changes
Neuroimaging plays a pivotal role in understanding catatonia among elderly patients. As age-related brain changes can complicate diagnosis, advanced imaging techniques like MRI and CT scans are invaluable tools. They help identify structural abnormalities that may underlie catatonic symptoms.
Studies indicate that older adults often exhibit distinct neuroanatomical variations compared to younger populations. These differences might manifest as atrophy in specific brain regions associated with movement and mood regulation, such as the basal ganglia or prefrontal cortex. Recognizing these patterns is crucial for differentiating between normal aging processes and pathological conditions.
Moreover, neuroimaging can reveal other coexisting medical issues impacting mental health, such as strokes or tumors. Such findings enhance our understanding of how multiple factors contribute to catatonia in older individuals.
Interpreting age-related brain changes requires expertise. Clinicians must consider both typical geriatric alterations and those indicative of psychiatric disorders when assessing elderly patients presenting with catatonic symptoms.
Adapting Diagnostic Criteria for Elderly Patients with Catatonic Symptoms
Adapting diagnostic criteria for elderly patients with catatonic symptoms is crucial, as traditional guidelines may not fully capture their unique needs. Older adults often present with atypical manifestations of catatonia. This can make diagnosis challenging and requires a tailored approach.
The DSM-5 outlines specific symptoms associated with catatonia, but these may overlap significantly with other geriatric conditions like dementia or delirium. Therefore, clinicians must consider the context in which symptoms arise and how they differ from typical presentations seen in younger populations.
Additionally, age-related changes in brain function can alter symptom expression. Clinicians should be aware that older patients might exhibit subtle signs of catatonia rather than overt behaviors commonly recognized in younger individuals.
Furthermore, cultural factors and historical medical treatment experiences also influence symptom presentation. Utilizing a comprehensive evaluation process allows healthcare providers to adapt existing criteria effectively while ensuring accurate diagnoses for this vulnerable population.
The Role of Comprehensive Geriatric Assessment in Catatonia Diagnosis
A Comprehensive Geriatric Assessment (CGA) plays a crucial role in diagnosing catatonia among elderly patients. This multifaceted evaluation goes beyond standard clinical assessments, incorporating various domains such as medical history, physical health, psychological status, and social circumstances. By examining these aspects holistically, clinicians can better identify the nuances of catatonic symptoms.
The CGA emphasizes understanding how comorbid conditions impact an individual’s mental state. For instance, underlying medical issues may contribute to or exacerbate catatonia symptoms. Identifying these relationships is vital for accurate diagnosis and effective treatment planning.
Moreover, a team approach is often employed during the CGA process. Involving geriatricians, psychiatrists, neurologists, and other specialists enhances diagnostic accuracy while ensuring that all potential factors are considered.
Additionally, CGAs facilitate ongoing communication with caregivers about observed behaviors and changes over time. This collaboration provides invaluable insights that aid in recognizing patterns associated with catatonic states in aging populations.
Caregiver Interviews: Gathering Crucial Information in Elderly Catatonia Cases
Caregiver interviews play a pivotal role in diagnosing catatonia in elderly patients. Caregivers often notice subtle changes in behavior that may go unreported during clinical assessments. Their observations can provide valuable context about the patient’s daily functioning and emotional state.
Engaging caregivers allows healthcare professionals to gather insights into any recent stressors, medication changes, or physical health issues impacting the patient. These details can illuminate patterns leading to catatonic symptoms, offering clues for accurate diagnosis.
Furthermore, caregivers can shed light on prior medical history and existing comorbidities that might contribute to the situation. This background helps clinicians differentiate between catatonia and other conditions like dementia or delirium.
Establishing open lines of communication with caregivers fosters a collaborative approach to treatment planning. By valuing their input, clinicians not only enhance diagnostic accuracy but also empower those who care for these vulnerable individuals.
Ethical Considerations in Diagnosing and Treating Catatonia in the Elderly
Diagnosing and treating catatonia in elderly patients raises several ethical considerations. Clinicians must navigate the complexities of informed consent, particularly if cognitive impairment is present. Understanding a patient’s capacity to make decisions about their treatment is crucial. Engaging with family members can help clarify patient preferences while respecting autonomy.
Another challenge involves balancing the risks and benefits of interventions. Some treatments may carry significant side effects, especially in older adults who often take multiple medications for comorbid conditions. Physicians need to weigh these potential harms against the possible improvements in quality of life.
Cultural sensitivity also plays a role when considering how different backgrounds perceive mental health issues. Patients’ beliefs and values should inform diagnostic approaches and treatment plans, ensuring care aligns with their expectations.
There’s an obligation to advocate for vulnerable populations like the elderly facing catatonic symptoms. Awareness of disparities in access to care is essential for promoting equitable treatment options across diverse communities.
Longitudinal Monitoring: Tracking Catatonic Symptoms in Aging Populations
Longitudinal monitoring of catatonic symptoms in aging populations is essential for accurate diagnosis and effective treatment. Regular follow-ups allow healthcare providers to observe changes over time, recognizing patterns that may indicate the progression or resolution of catatonia. This ongoing assessment can also highlight responses to interventions, helping clinicians fine-tune treatment plans tailored specifically for elderly patients.
Maintaining detailed records during these evaluations ensures that subtle shifts in behavior or cognition do not go unnoticed. Such tracking enables caregivers and medical professionals alike to distinguish between transient episodes and persistent conditions. Additionally, it fosters a collaborative approach among multidisciplinary teams focused on geriatric mental health.
Understanding the dynamics of catatonia requires patience and vigilance. By implementing systematic observation protocols, we can better navigate the complexities associated with diagnostic challenges in elderly patients with catatonic symptoms. This comprehensive strategy enhances care quality while promoting healthier outcomes for our aging population facing this often-overlooked condition.