Introduction to the Dopamine Hypothesis in Catatonia
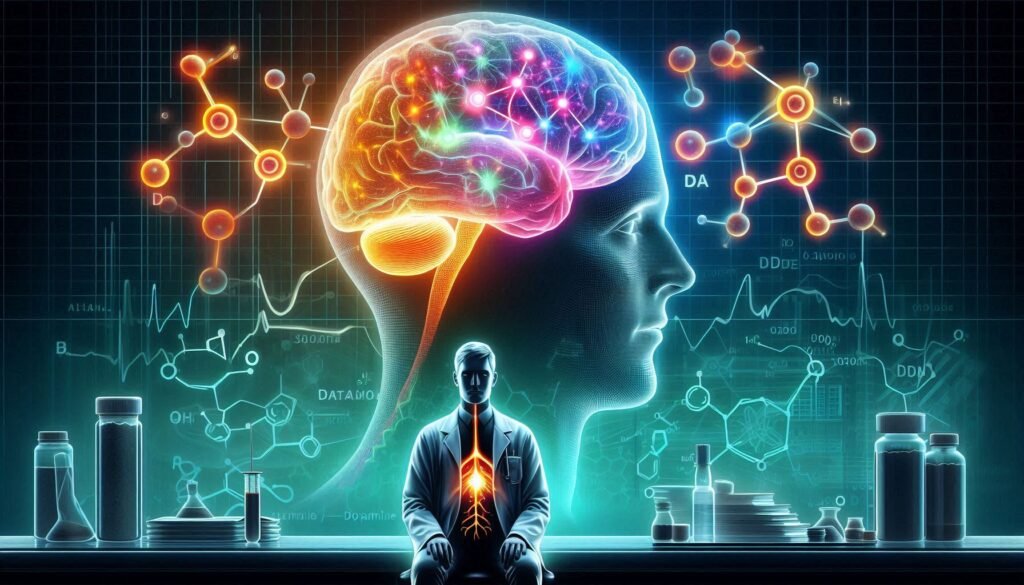
Catatonia is a complex and often misunderstood condition that manifests through various symptoms, including immobility, excessive movement, or altered consciousness. Despite its diverse presentations, researchers have increasingly focused on the role of dopamine—a neurotransmitter crucial for regulating mood and movement. This focus has given rise to what’s known as the Dopamine Hypothesis in Catatonia.
Understanding how dopamine contributes to catatonic symptoms can unravel many mysteries surrounding this disorder. By exploring dopamine pathways, receptor abnormalities, and even genetic factors at play, we gain valuable insights into potential treatments and interventions. With advancements in neuroimaging techniques and pharmacological research shedding light on this hypothesis, there’s much to discuss about its implications for both clinical practice and future studies.
Join us as we delve deeper into the current understanding of the Dopamine Hypothesis in Catatonia—an exploration that not only aims to clarify existing knowledge but also sparks new conversations around effective management strategies for those affected by this challenging condition.
Dopamine Pathways Involved in Catatonic Symptoms
Dopamine pathways play a crucial role in the manifestation of catatonic symptoms. The mesolimbic and mesocortical pathways are particularly significant, as they connect the brain’s reward system to areas governing cognition and motor activity. Disruptions within these circuits can lead to abnormal behavior often seen in catatonia.
The striatum is another key region influenced by dopamine activity. It integrates input from various cortical areas, affecting movement regulation and emotional responses. When dopamine transmission is impaired here, it may result in reduced motor output or increased rigidity.
Additionally, the nigrostriatal pathway links dopamine production directly to voluntary movements. Alterations within this pathway can contribute to akinesia—a common feature of catatonia where patients exhibit a lack of spontaneous movement.
Understanding these pathways not only sheds light on the biological underpinnings of catatonia but also opens avenues for targeted interventions aimed at restoring normal dopaminergic function.
Dopamine Receptor Abnormalities in Catatonic States
Dopamine receptor abnormalities play a crucial role in understanding catatonia. These receptors are integral to how dopamine transmits signals within the brain, influencing mood, behavior, and motor control. In individuals experiencing catatonic states, research has shown alterations in these receptors that may contribute to their symptoms.
One significant finding is the dysregulation of D2 dopamine receptors. Studies suggest that increased sensitivity or density of these receptors can lead to heightened dopaminergic activity. This excessive activation might be linked to psychomotor agitation and other forms of abnormal movement seen in catatonia.
Additionally, there’s evidence pointing toward a deficiency in D1 receptor function. Such deficits may hinder proper signaling pathways associated with motivation and voluntary movement, resulting in the immobility often observed during catatonic episodes.
Understanding these receptor dynamics enhances our grasp of how disruptions in dopamine signaling translate into clinical manifestations. Ongoing research continues to explore this complex relationship further as scientists aim for more effective therapeutic strategies.
Neuroimaging Evidence Supporting the Dopamine Hypothesis
Neuroimaging studies have emerged as a pivotal tool in exploring the dopamine hypothesis in catatonia. Advanced techniques like functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) allow researchers to visualize brain activity and neurotransmitter levels in real time.
Findings consistently show altered dopaminergic function in individuals with catatonic symptoms. For instance, reduced dopamine receptor binding has been linked to motor deficits typically observed during catatonic episodes. These changes suggest that dysregulation of dopamine pathways plays a critical role in the onset of these symptoms.
Moreover, neuroimaging has provided insights into specific brain regions involved. The striatum, which is rich in dopaminergic neurons, often shows abnormal activation patterns during catatonia. This area’s involvement highlights its significance for understanding movement-related disturbances associated with this condition.
Additionally, longitudinal studies indicate that therapeutic interventions targeting dopamine receptors can lead to observable changes on neuroimaging scans. Such evidence reinforces the notion that addressing dopaminergic dysfunction could be beneficial for those experiencing catatonia.
Pharmacological Studies and Dopamine in Catatonia
Pharmacological studies have become crucial in understanding the role of dopamine in catatonia. Various antipsychotic medications target dopamine receptors, showcasing how these drugs can alleviate certain symptoms associated with catatonic states. The response to dopaminergic agents provides insight into the underlying pathophysiology.
Research indicates that patients experiencing catatonia often benefit from benzodiazepines and atypical antipsychotics. These treatments suggest an imbalance in dopamine signaling may be a significant factor contributing to catatonia. By modulating this neurotransmitter system, clinicians can help restore normal function and improve patient outcomes.
Additionally, some studies highlight that rapid-acting interventions like ketamine could offer promise for treatment-resistant cases of catatonia. Ketamine’s unique interaction with NMDA receptors also demonstrates the complexity of neurotransmitter systems involved.
The nuances of pharmacotherapy underscore the importance of tailoring treatments based on individual responses to dopaminergic manipulation. Ongoing research continues to refine our understanding and potentially enhance therapeutic strategies for managing this challenging condition.
Genetic Factors Influencing Dopamine Function in Catatonia
Genetic factors play a crucial role in influencing dopamine function, particularly in relation to catatonia. Various genes are involved in the synthesis, transport, and receptor activity of dopamine. For instance, genetic variations can affect the production of enzymes responsible for dopamine metabolism.
Polymorphisms within the COMT gene impact how efficiently dopamine is broken down. This can lead to altered levels of neurotransmitter availability, potentially exacerbating catatonic symptoms. Variations in other genes related to dopaminergic pathways have also been associated with increased susceptibility to these states.
Moreover, certain inherited traits may predispose individuals to develop disorders characterized by catatonia. Family studies reveal that several psychiatric conditions linked with dysregulated dopamine function often cluster together within families.
Understanding these genetic underpinnings is essential for developing targeted treatments and interventions. As research progresses, it may provide insights into personalized approaches tailored to individual genetic profiles affecting dopamine dynamics.
Dopamine’s Interaction with Other Neurotransmitters
Dopamine does not exist in isolation; it interacts with various other neurotransmitters that play a critical role in regulating mood and behavior. One of the most significant interactions is with serotonin. This relationship can influence emotional states, potentially impacting catatonic symptoms.
Another important interaction occurs between dopamine and gamma-aminobutyric acid (GABA). GABA acts as an inhibitory neurotransmitter, balancing excitatory signals. Alterations in this balance may contribute to the motor disturbances seen in catatonia.
Glutamate also plays a vital role alongside dopamine. As the primary excitatory neurotransmitter, glutamate’s interaction can affect synaptic plasticity and overall brain function. Dysregulation here might exacerbate catatonic features.
Moreover, recent studies suggest that norepinephrine could modulate dopaminergic pathways too. The interplay among these neurotransmitters highlights the complexity behind catatonic disorders and emphasizes the need for integrated approaches to treatment strategies.
Challenges to the Dopamine Hypothesis in Catatonia
The Dopamine Hypothesis in Catatonia is not without its challenges. Critics argue that catatonia cannot be solely explained by dopamine dysregulation. Some patients exhibit symptoms despite normal dopamine levels, suggesting other mechanisms may also play a role.
Additionally, the complexity of catatonic disorders complicates the interpretation of findings. Variability in symptoms among individuals raises questions about whether a single neurotransmitter can account for such diversity in clinical presentation.
Research identifying only certain subtypes of dopamine receptors implicated in specific aspects of catatonia further complicates this hypothesis. This highlights the need to consider alternative pathways and neurotransmitters involved.
Moreover, some studies point to environmental factors or stressors as significant contributors to catatonic states, challenging the notion that biological underpinnings are predominant. Understanding these interactions is crucial for refining our approach to treatment and diagnosis within this complex disorder.
Clinical Implications of the Dopamine Hypothesis
Understanding the dopamine hypothesis in catatonia has significant clinical implications. Clinicians can better identify and treat patients exhibiting catatonic symptoms by recognizing the role of dopamine dysfunction. This insight allows for targeted interventions that address underlying neurochemical imbalances rather than merely managing symptoms.
Pharmacological treatments focusing on dopaminergic pathways may provide effective relief for those suffering from catatonia. Medications such as benzodiazepines or antipsychotics have shown promise in alleviating these symptoms, reinforcing the importance of understanding dopamine’s role.
Furthermore, awareness of this hypothesis encourages a more comprehensive approach to patient assessment. Evaluating neurotransmitter function could enhance diagnostic accuracy and lead to tailored treatment plans designed specifically for individual needs.
Research into this area fosters collaboration among clinicians, neuroscientists, and psychologists. Such partnerships are crucial for developing innovative therapies that target specific neurotransmitter systems involved in catatonia while advancing our overall comprehension of mental health disorders.
Future Research Directions in Dopamine and Catatonia
Future research on the dopamine hypothesis in catatonia holds significant promise for advancing our understanding of this complex condition. As studies continue to explore the intricate relationship between dopamine pathways and catatonic symptoms, a few key areas warrant attention.
More extensive genetic research could illuminate how individual differences in dopamine function contribute to varying presentations of catatonia. Identifying specific genetic markers may pave the way for personalized treatment approaches tailored to an individual’s neurochemical profile.
Integrating advanced neuroimaging techniques can enhance our comprehension of dopamine receptor dynamics in real time. This would provide valuable insights into how these receptors fluctuate during different emotional states or therapeutic interventions.
Moreover, exploring other neurotransmitter systems that interact with dopamine will be crucial for developing comprehensive treatment strategies. The interplay between serotonin, glutamate, and GABA deserves further investigation as it may uncover additional layers influencing catatonic behavior.
Clinical trials focusing on novel pharmacological agents targeting specific dopamine pathways could revolutionize treatment options for those suffering from catatonia. By examining the efficacy of new treatments alongside traditional therapies, researchers can identify which combinations yield optimal results.
Emphasizing collaborative efforts among neuroscientists, psychiatrists, and clinicians will be vital as we move forward in unraveling the complexities surrounding the dopamine hypothesis in catatonia. These efforts may ultimately improve outcomes for patients grappling with this challenging condition.