Catatonia is a complex neuropsychiatric condition that can leave individuals in a state of unresponsiveness, rigidity, or extreme agitation. For many patients grappling with this debilitating disorder, traditional treatments may fall short. Enter Electroconvulsive Therapy (ECT)—a powerful intervention that has emerged as a lifeline for those experiencing severe catatonia. This innovative treatment harnesses the brain’s electrical activity to alleviate symptoms and restore functionality.
In the following sections, we will explore the intricate relationship between ECT and catatonia, delving into its efficacy and procedures. We’ll examine how ECT works at a neurobiological level and what makes it an essential option for many patients. Whether you’re seeking information for yourself or someone you care about, understanding Electroconvulsive Therapy in Catatonia: Procedures and Outcomes could pave the way toward recovery and renewed hope.
Understanding ECT: A Powerful Treatment for Severe Catatonia
Electroconvulsive Therapy (ECT) is a medical treatment primarily used for severe mental health conditions, including catatonia. Characterized by its ability to provoke controlled seizures through electrical stimulation of the brain, ECT can significantly alleviate symptoms when other treatments fail.
For individuals with catatonia, symptoms may present as extreme withdrawal or abnormal motor activity. These manifestations severely impair daily functioning and quality of life. ECT offers rapid relief by targeting key areas in the brain responsible for mood regulation and movement.
The procedure typically involves several sessions conducted under general anesthesia, ensuring patient comfort and safety throughout the process. The exact mechanism behind ECT’s effectiveness remains complex but is believed to promote neuroplasticity—the brain’s ability to reorganize itself—which can lead to significant improvements in symptom severity.
Research shows that many patients experience substantial recovery following ECT treatment, often leading to restored normalcy in their lives. As awareness grows about its efficacy, more individuals are considering this powerful option for combating severe catatonia.
The Neurobiological Basis of ECT’s Efficacy in Catatonia
Electroconvulsive Therapy (ECT) has long been recognized for its efficacy in treating severe mental health conditions, particularly catatonia. The neurobiological mechanisms behind its effectiveness are complex and multifaceted. ECT induces a controlled seizure that seems to reset neural circuits involved in mood regulation.
One key aspect of ECT’s action is the modulation of neurotransmitters, including serotonin, norepinephrine, and dopamine. This alteration can help alleviate symptoms associated with catatonia by rebalancing brain chemistry.
Additionally, research indicates that ECT enhances neuroplasticity—the brain’s ability to adapt and reorganize itself. This adaptive capacity allows individuals experiencing catatonia to potentially regain functional connections disrupted during their illness.
Moreover, structural changes in the brain have been observed post-ECT treatment. These changes may contribute to improved emotional regulation and reduced rigidity often seen in patients suffering from catatonic states, underscoring ECT’s role as a powerful therapeutic intervention.
Pre-ECT Evaluation: Determining Candidacy for the Procedure
Before initiating Electroconvulsive Therapy (ECT) in catatonia, a thorough pre-ECT evaluation is essential to determine candidacy. This assessment typically involves a comprehensive psychiatric evaluation and medical history review. Clinicians must evaluate the severity of catatonic symptoms, duration of illness, and previous treatment responses.
It’s crucial to identify any coexisting medical conditions that may complicate ECT administration. Patients with cardiovascular problems or significant neurological disorders require special consideration. The potential for adverse reactions must be carefully weighed against the benefits of treatment.
Additionally, informed consent plays a vital role in this process. Patients should understand what ECT entails, including possible side effects and expected outcomes. Adequate communication helps alleviate fears and ensures patient cooperation during treatment.
Family involvement can also enhance decision-making during this phase. They can provide insights into the patient’s condition while offering support throughout the journey toward recovery from catatonia through ECT.
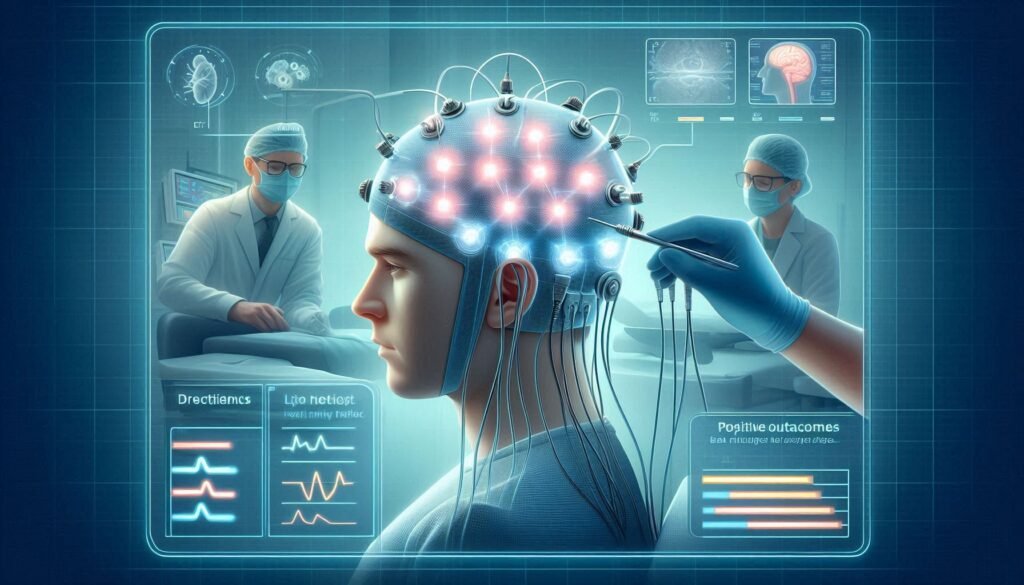
ECT Administration: Step-by-Step Procedure in Catatonic Patients
Electroconvulsive Therapy (ECT) administration in catatonic patients follows a careful, structured approach. First, the patient undergoes a comprehensive medical evaluation to ensure they are physically fit for the procedure. This includes monitoring vital signs and assessing any existing health conditions that may affect treatment.
Once deemed suitable, the patient is taken to a specialized ECT suite where they receive an intravenous line for sedation and muscle relaxants. An anesthesiologist administers general anesthesia to ensure comfort during the procedure.
After achieving proper anesthesia, electrodes are placed on specific areas of the scalp. The placement can vary based on individual needs but typically involves either bilateral or unilateral positioning.
The clinician then delivers controlled electrical pulses through these electrodes, inducing a brief seizure lasting 30-60 seconds. Monitoring continues throughout this process to assess physiological responses and ensure patient safety at all times.
Frequency and Duration: Optimizing ECT Treatment Protocols
The frequency and duration of Electroconvulsive Therapy (ECT) are crucial for maximizing its effectiveness in treating catatonia. Typically, ECT sessions occur two to three times a week. This schedule allows the brain to respond positively while minimizing potential fatigue from excessive stimulation.
Duration also plays a vital role. Most treatment courses last between six to twelve sessions, depending on individual patient needs and response rates. Clinicians often tailor these protocols based on how quickly symptoms improve or if any side effects emerge.
During initial phases, close monitoring is essential. Healthcare providers assess both clinical progress and tolerability after each session, making adjustments as needed. Adapting the protocol ensures optimal outcomes tailored specifically for patients battling severe catatonia.
Research indicates that longer-lasting remission may be achieved with carefully timed follow-up treatments post-initial course completion. Regular assessments ensure ongoing efficacy while balancing safety in managing this delicate mental health condition effectively.
Immediate and Long-Term Outcomes of ECT in Catatonia
Electroconvulsive Therapy (ECT) can lead to significant improvements in patients experiencing catatonia. Immediate outcomes are often observed within a few sessions, with many individuals showing reduced motor symptoms and enhanced responsiveness. This rapid alleviation is crucial, especially as catatonic states can severely impair daily functioning.
Long-term outcomes reflect the robustness of ECT’s effectiveness. Many patients experience sustained remission from catatonic features for months or even years following treatment. The likelihood of full recovery increases when ECT is combined with appropriate pharmacological interventions.
However, it’s essential to monitor patients over time as relapse may occur in some cases. Regular follow-ups help track mental health status and ensure timely re-intervention if needed.
The multi-faceted benefits of ECT extend beyond symptom relief; improved quality of life has been reported by numerous recipients after their therapy course concludes. Their capacity to engage socially and return to everyday activities often enhances dramatically post-treatment.
Managing Side Effects: Cognitive and Physical Considerations
Electroconvulsive Therapy (ECT) can be a lifesaving intervention for individuals suffering from catatonia, but it does come with potential side effects. Understanding these is crucial for both patients and caregivers. Cognitive effects, such as confusion or memory loss, may occur shortly after treatment. These symptoms often resolve over time but can be distressing during recovery.
Physical side effects are also worth noting. Patients might experience headaches, muscle soreness, or nausea following ECT sessions. While generally mild, these issues can impact the overall comfort level of the individual receiving treatment.
Managing cognitive side effects typically involves supportive care and patience. Engaging in mental exercises may help restore cognitive function more quickly post-treatment.
For physical discomforts like headache or nausea, simple interventions such as hydration and rest can significantly enhance patient well-being. Open communication with healthcare providers remains essential to address any concerns that arise during this critical phase of recovery.
Combining ECT with Pharmacological Treatments: Synergistic Approaches
Combining Electroconvulsive Therapy (ECT) with pharmacological treatments can significantly enhance treatment outcomes for patients experiencing catatonia. This approach allows clinicians to tailor therapy according to individual needs, addressing both acute symptoms and underlying neurobiological factors.
Antidepressants, antipsychotics, or mood stabilizers may be used alongside ECT to optimize patient care. The synergy between these medications and electroconvulsive therapy often leads to quicker symptom relief while potentially reducing the overall number of ECT sessions required.
Monitoring is essential when integrating medication with ECT. Adjustments in dosage might be necessary as the patient’s condition improves or stabilizes. Careful evaluation ensures that side effects are managed effectively while maximizing therapeutic benefits.
Research suggests that such combinations not only improve short-term outcomes but also promote long-lasting recovery from catatonia. By employing a multifaceted treatment strategy, healthcare providers can better support patients on their journey toward mental wellness.
ECT vs. Other Treatments: Comparative Efficacy in Catatonia
Electroconvulsive Therapy (ECT) stands out among various treatment options for catatonia due to its rapid and profound effects. Unlike conventional antidepressants or antipsychotics, which may take weeks to show benefits, ECT can often yield significant improvements within days. This swift action is particularly crucial in severe cases where timely intervention is essential.
Research indicates that ECT has a higher response rate compared to pharmacological treatments alone. A substantial percentage of patients with catatonia experience remission after a series of ECT sessions, making it a preferred choice when traditional methods fail or are inadequate.
Other therapies like psychotherapy have limited efficacy in addressing the acute symptoms of catatonia. While helpful for long-term management and underlying issues, they do not provide the immediate relief that many patients require during episodes.
Moreover, combining ECT with medications can enhance treatment outcomes further. By leveraging both approaches simultaneously, clinicians may optimize patient recovery from this challenging condition effectively.
Post-ECT Care: Ensuring Sustained Recovery from Catatonia
Post-ECT care is crucial for ensuring long-term recovery from catatonia. After undergoing Electroconvulsive Therapy (ECT), patients often require comprehensive support to maintain their progress. This phase includes close monitoring of mental health, medication adjustments, and ongoing therapy sessions.
Continued psychiatric follow-up helps identify any potential relapses early. Regular appointments allow healthcare providers to adjust treatment plans based on the patient’s evolving needs. Support groups can also be invaluable, providing a community where individuals share experiences and coping strategies.
Family involvement plays a significant role in post-ECT recovery as well. Educating family members about catatonia and ECT can foster understanding and create a supportive environment at home. Engaging with loved ones helps reduce feelings of isolation.
Lifestyle changes may further enhance recovery outcomes too. Encouraging healthy habits—such as regular exercise, balanced nutrition, and adequate sleep—can significantly boost overall well-being. Mindfulness practices or meditation can also serve as effective tools for managing stress.
Sustained engagement with treatment resources improves chances of lasting stability after ECT for catatonia patients. By prioritizing ongoing care and support systems, individuals are better equipped to navigate their journey towards wellness successfully.