Catatonia is a complex and often misunderstood condition that can significantly impact an individual’s mental health. Characterized by a range of symptoms, including immobility, mutism, and unusual posturing, catatonia often leaves both patients and caregivers searching for effective treatment options. Among the various approaches available, benzodiazepines have emerged as first-line treatments for managing this challenging disorder. Known for their calming effects on the central nervous system, these medications offer hope to those struggling with catatonic symptoms.
In this blog post, we will explore the efficacy of benzodiazepines in treating catatonia—examining their mechanisms of action, dosage guidelines, success rates in alleviating symptoms, potential side effects, and how they can be integrated into long-term care strategies. Whether you are a healthcare professional or someone seeking to understand more about this condition and its management options, you’ll find valuable insights that illuminate the role of benzodiazepines in addressing catatonia effectively.

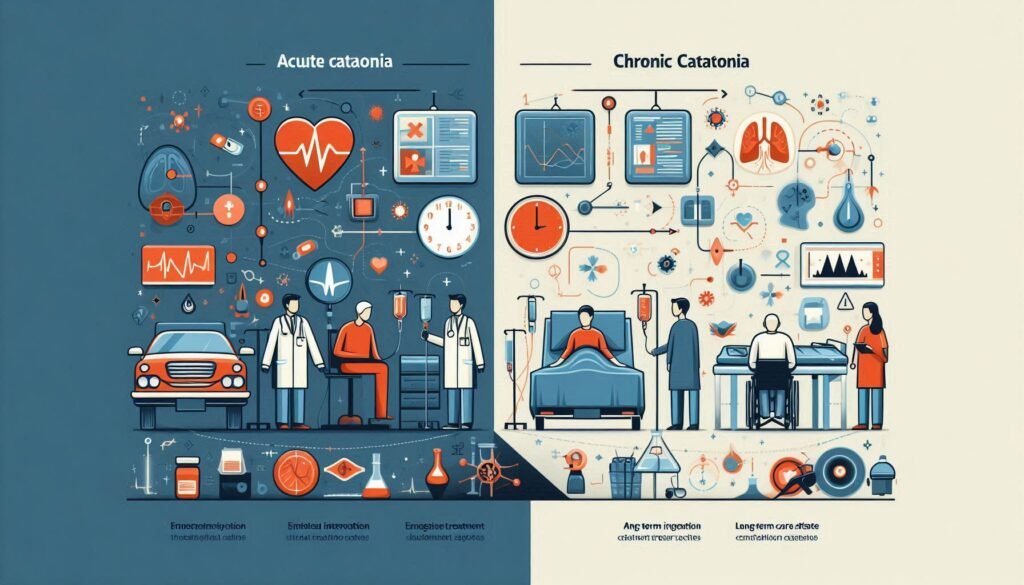
Understanding Catatonia: A Brief Overview of the Condition
Catatonia is a neuropsychiatric syndrome characterized by abnormal motor behavior and altered mental states. It can manifest as extreme agitation, stupor, or even unresponsiveness. Patients may exhibit unusual postures or repetitive movements, which can be distressing for both the individual and their loved ones.
Historically linked to schizophrenia, catatonia can occur in various settings, including mood disorders, medical illnesses, and substance use. Its symptoms often overlap with other psychiatric conditions, making diagnosis challenging for healthcare providers.
The onset of catatonic features may happen suddenly or gradually. This unpredictability adds complexity to treatment approaches. Due to its varied presentations, early recognition is crucial for effective management.
While once thought rare, recent studies suggest that catatonia might be more common than previously acknowledged. Understanding this condition paves the way for exploring targeted treatments like benzodiazepines that play a vital role in alleviating symptoms and improving patient outcomes.
The Role of Benzodiazepines as First-Line Treatment for Catatonia
Benzodiazepines play a crucial role as first-line treatments for catatonia, a neuropsychiatric syndrome characterized by immobilization and abnormal motor behaviors. These medications are often the initial choice due to their rapid onset of action and effectiveness in alleviating symptoms.
Catatonia can occur in various psychiatric conditions, including schizophrenia, mood disorders, and medical illnesses. Patients may present with mutism, stupor, or bizarre posturing. Benzodiazepines address these symptoms effectively by enhancing GABA (gamma-aminobutyric acid) activity in the brain.
The ease of administration also makes benzodiazepines appealing for acute situations. They can be given orally or intravenously based on the severity of symptoms and patient needs. This flexibility allows healthcare providers to tailor treatment plans specifically for each individual.
In addition to being effective alone, benzodiazepines may prepare patients for further therapeutic interventions like psychotherapy or electroconvulsive therapy (ECT). Their use marks an essential step in managing this complex condition efficiently.
Mechanism of Action: How Benzodiazepines Work in Catatonic Patients
Benzodiazepines are widely recognized for their sedative properties, playing a crucial role in the management of catatonia. Their primary mechanism involves enhancing the effect of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits neuronal activity. This increase in GABAergic transmission leads to reduced excitability within the central nervous system.
In catatonic patients, this enhanced inhibitory action can alleviate symptoms like rigidity and stupor. By promoting relaxation and reducing hyperactivity in neural circuits, benzodiazepines help restore some level of normal functioning.
Additionally, these medications may assist with mood stabilization and anxiety reduction, which can be particularly beneficial for individuals experiencing co-occurring psychiatric conditions. The rapid onset of action makes them suitable when immediate intervention is needed.
The precise neurobiological pathways remain complex; however, it’s clear that benzodiazepines provide significant symptomatic relief for those enduring catatonia by modulating brain chemistry effectively.
Types of Benzodiazepines Used in Catatonia Treatment
Benzodiazepines are a class of medications frequently employed in the treatment of catatonia. Their effectiveness largely depends on their specific properties and how they interact with patients’ symptoms. Several types stand out in clinical practice.
Lorazepam is often the first choice for treating catatonia due to its rapid action and efficacy. It can be administered intravenously, allowing for swift relief of symptoms, especially in acute situations. This makes it ideal for hospitalized patients who need immediate intervention.
Diazepam, another well-known benzodiazepine, is also used but less frequently than lorazepam. Its longer half-life means it may not provide as quick a response but can be beneficial for ongoing management once initial stabilization occurs.
Midazolam is yet another option, known for its short duration and potency. It’s typically reserved for cases requiring continuous sedation or when other treatments have failed to yield results effectively.
Dosage and Administration: Guidelines for Benzodiazepine Use in Catatonia
When treating catatonia with benzodiazepines, proper dosage and administration are crucial. Initial doses usually start low to minimize side effects while assessing the patient’s response. A typical starting dose might range from 5 to 10 mg of lorazepam administered orally or intravenously.
Frequency of administration often depends on severity. For acute situations, intravenous delivery may be preferred for rapid effect. Some patients may require doses every few hours until symptoms improve significantly.
Continuous monitoring is essential during treatment. Adjustments in dosage can occur based on individual tolerance and responsiveness. Physicians must evaluate efficacy regularly to ensure optimal outcomes without unnecessary sedation.
In chronic cases, transitioning from high-dose acute treatment to a maintenance regimen is common. This approach helps manage symptoms over time while reducing risks associated with prolonged high-dosage use of benzodiazepines in catatonic patients.
Efficacy Rates: Success of Benzodiazepines in Treating Catatonic Symptoms
Benzodiazepines have shown promising efficacy rates in treating catatonia. Studies indicate that around 60% to 80% of patients respond positively to these medications. This response often manifests as a significant reduction in catatonic symptoms, such as immobility or mutism.
The rapid action of benzodiazepines is one reason behind their success. Many patients experience noticeable improvements within hours or days after initiation of treatment. This quick onset can be crucial for individuals facing severe distress due to catatonia.
However, not all patients will achieve the same level of benefit from benzodiazepine therapy. Factors like the underlying cause of catatonia and individual patient characteristics play a role in determining effectiveness.
Long-term studies also underscore the importance of monitoring response rates over time, ensuring that treatment remains tailored to each patient’s needs. Continued assessment helps optimize outcomes and manage any potential complications associated with prolonged use.
Time to Response: What to Expect When Using Benzodiazepines
When treating catatonia with benzodiazepines, the time to response can vary significantly among patients. Many individuals start noticing improvements within hours of administration, especially when given intravenously. This rapid onset is one reason benzodiazepines are favored as a first-line treatment.
However, not everyone will respond immediately. Some might take several days before any noticeable changes occur in their symptoms. Healthcare providers typically monitor patients closely during this period to adjust dosages or explore other options if necessary.
The initial response often hinges on factors like the severity of catatonia and individual patient characteristics. Age, overall health, and previous treatments can all influence how quickly someone responds to benzodiazepines.
It’s essential for caregivers and family members to remain patient during this process. Open communication with healthcare professionals will help ensure that adjustments are made as needed while providing support for the affected individual throughout their recovery journey.
Potential Side Effects and Risks of Benzodiazepine Treatment
Benzodiazepines are often a go-to treatment for catatonia, but they come with potential side effects. Patients may experience sedation, dizziness, or confusion shortly after administration. These symptoms can interfere with daily functioning and increase the risk of falls.
Long-term use raises concerns around dependence and withdrawal symptoms. As patients become accustomed to the medication, their bodies may require higher doses to achieve the same effects. This tolerance can complicate treatment plans and lead to challenging situations when trying to discontinue use.
Cognitive impairment is another significant concern. Some individuals might find it difficult to concentrate or remember things while on benzodiazepines. This cognitive fog can impact quality of life in various ways.
Additionally, interactions with other medications pose risks that should be closely monitored by healthcare professionals. Combining benzodiazepines with substances like alcohol or opioids heightens the danger of respiratory depression and overdose—a serious medical emergency requiring immediate attention.
Combining Benzodiazepines with Other Treatments: Synergistic Approaches
Combining benzodiazepines with other treatments can enhance the management of catatonia. This multifaceted approach allows for a more comprehensive strategy to address the complex symptoms associated with the condition.
Antipsychotics are often used alongside benzodiazepines, especially in cases where psychotic features coexist. These medications can help stabilize mood and alleviate psychotic symptoms, potentially leading to a quicker recovery from catatonic states.
Electroconvulsive therapy (ECT) is another option that may be combined with benzodiazepine treatment. ECT has shown effectiveness in severe cases of catatonia, particularly when rapid response is necessary. The synergy between these therapies can yield better outcomes than either method alone.
Psychotherapy also plays a vital role in ongoing care. While not typically first-line for acute episodes, integrating therapeutic interventions post-stabilization supports emotional processing and helps prevent future episodes of catatonia or related disorders.
Long-Term Management: Benzodiazepines in Ongoing Catatonia Care
Long-term management of catatonia often involves a careful and strategic approach to treatment. Benzodiazepines play a pivotal role in this ongoing care, particularly due to their rapid action and effectiveness in alleviating acute symptoms. However, managing long-term use requires vigilance.
Patients receiving benzodiazepines for prolonged periods may develop tolerance or dependence. Regular assessments are essential to evaluate the necessity of continuing these medications. Health professionals should monitor patients closely for any signs of side effects or diminishing efficacy.
In many cases, combining benzodiazepines with psychotherapy or other pharmacological treatments can enhance overall outcomes. This integrative strategy helps address not just the immediate symptoms but also underlying causes contributing to catatonic episodes.
Regular follow-ups with healthcare providers help ensure that each patient’s treatment plan remains tailored to their evolving needs. Education about potential risks and benefits empowers patients and families, fostering better adherence to prescribed regimens.
Managing catatonia is complex, yet with appropriate strategies involving benzodiazepines and supportive therapies, it is possible for individuals affected by this condition to achieve a better quality of life. Ongoing research continues to refine our understanding of effective long-term solutions, offering hope for improved care methods in the future.