Introduction to the Gut-Brain Axis in Catatonia
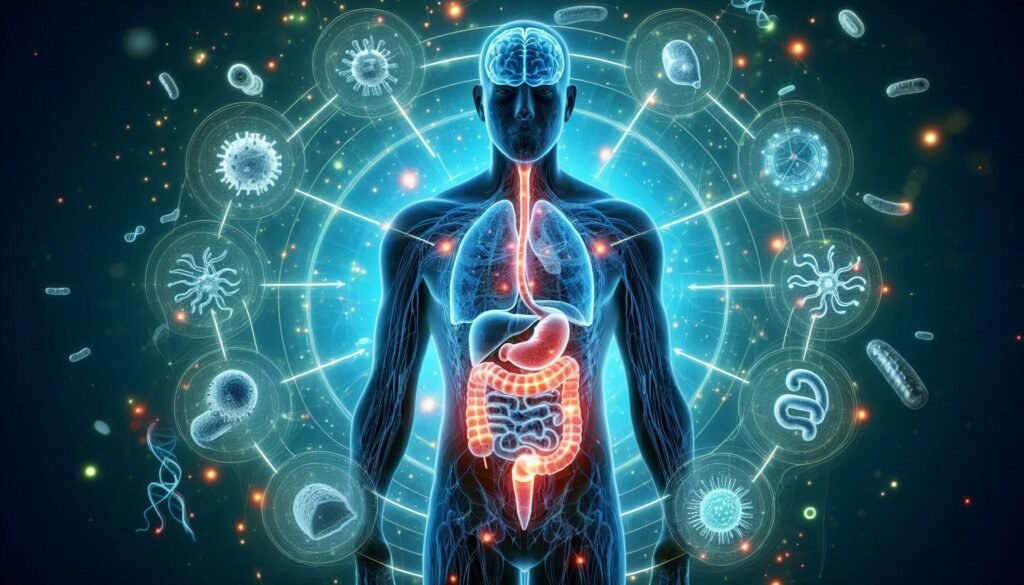
The gut-brain axis is a fascinating and complex communication network that links our digestive system to our brain. Recent research has brought this connection into the spotlight, especially regarding its role in mental health disorders. One area of particular interest is catatonia—a condition characterized by a range of symptoms including immobility, rigidity, and altered consciousness.
Understanding the role of the gut-brain axis in catatonic states could unlock new avenues for treatment and management strategies. Our gut houses trillions of microorganisms that influence not just digestion but also mood, cognition, and behavior. Dysbiosis or an imbalance in these microbes may play a crucial part in the development or exacerbation of catatonic symptoms.
As we delve deeper into this emerging field, we’ll uncover how factors like inflammation, neurotransmitter production, and even dietary choices can impact both gut health and mental well-being. Join us on this intriguing journey as we explore how understanding the role of the gut-brain axis might reshape our approach toward managing catatonia effectively.
Microbiome Dysbiosis and Its Impact on Catatonic Symptoms
The human gut is home to trillions of microorganisms, collectively known as the microbiome. These microbes play a crucial role in maintaining overall health, including mental well-being. Microbiome dysbiosis occurs when this balance is disrupted, leading to potential negative effects on various bodily functions.
Research suggests that dysbiosis may contribute to catatonic symptoms by altering neurotransmitter production and inflammatory responses. An imbalance in gut bacteria can lead to reduced levels of serotonin and GABA, both essential for mood regulation and cognitive function. This alteration might exacerbate or trigger catatonia.
Moreover, the inflammation caused by dysbiosis can affect communication between the gut and brain. When harmful bacteria proliferate, they release toxins that may damage neural pathways critical for movement and cognition. This disruption could manifest as motor disturbances commonly seen in catatonic presentations.
Understanding how microbiome dysbiosis impacts these symptoms opens new avenues for therapeutic approaches targeting gut health as a means of addressing catatonic states.
Gut Inflammation and Blood-Brain Barrier Integrity in Catatonia
Gut inflammation plays a significant role in the health of the blood-brain barrier (BBB). This protective shield separates the brain from harmful substances circulating in the bloodstream. When inflammation occurs within the gut, it can trigger systemic responses that compromise BBB integrity.
Dysregulated immune responses often lead to an influx of inflammatory cytokines into circulation. These molecules may disrupt tight junctions between endothelial cells in the BBB. As a result, this disruption allows toxins and pathogens to reach neural tissue, potentially triggering catatonic symptoms.
Research indicates that individuals experiencing catatonia often display markers of increased gut permeability or “leaky gut.” This condition can exacerbate neuroinflammation and further impair cognitive function. Understanding these connections is crucial for developing effective interventions.
Restoring intestinal health may help reinforce BBB integrity and mitigate some catatonic presentations. Future studies should investigate targeted therapies aimed at reducing gut inflammation as potential strategies for managing catatonia more effectively.
Neurotransmitter Production in the Gut and Catatonia
The gut is often called the “second brain” due to its complex network of neurons and its ability to produce neurotransmitters. In fact, around 90% of serotonin, a key neurotransmitter associated with mood regulation, is synthesized in the gastrointestinal tract. This production underscores the significant role of gut health in mental well-being.
When dysbiosis occurs—an imbalance in the gut microbiome—it can disrupt this delicate balance of neurotransmitter synthesis. Such disturbances are linked to various psychiatric conditions, including catatonia. The lack of necessary bacteria may lead to reduced levels of serotonin and other crucial chemicals that influence mood and behavior.
Moreover, gamma-aminobutyric acid (GABA), another important neurotransmitter produced in the gut, helps regulate anxiety and stress responses. A deficiency in GABA could potentially heighten susceptibility to catatonic states or exacerbate existing symptoms.
Understanding how these neurotransmitters function within the context of catatonia highlights an intricate connection between our digestive system and mental health. Research continues to explore how optimizing gut health might impact neurological outcomes positively.
The Vagus Nerve: Connecting Gut and Brain in Catatonic States
The vagus nerve plays a critical role in the communication between the gut and brain, particularly in catatonic states. As one of the longest cranial nerves, it stretches from the brainstem to various organs, including those in the gastrointestinal tract. This intricate connection is vital for regulating bodily functions such as heart rate and digestion.
Research indicates that vagal tone can influence mood and behavior. When there’s dysfunction within this pathway, it may contribute to symptoms seen in catatonia. A disrupted vagal response could impair emotional regulation, leading to withdrawal or immobility often associated with these states.
Moreover, signals sent through the vagus nerve can affect inflammation levels throughout the body. Increased inflammation has been linked to several psychiatric disorders, suggesting that it might play a role in triggering catatonic episodes.
Understanding how this nerve operates opens up potential avenues for therapeutic interventions aimed at restoring balance between gut health and mental well-being through targeted stimulation techniques or dietary approaches.
Gut Metabolites and Their Influence on Catatonia Development
Gut metabolites play a crucial role in influencing brain function and behavior. These small molecules are produced during the fermentation of dietary fibers by gut microbiota. Their impact on mental health cannot be overstated, especially in relation to catatonic states.
Short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate are key players among gut metabolites. They help maintain the integrity of the blood-brain barrier and modulate neuroinflammation. When SCFA levels drop due to dysbiosis, it could lead to altered cognitive functions associated with catatonia.
Moreover, certain amino acids derived from gut bacteria affect neurotransmitter synthesis. For example, tryptophan is essential for serotonin production; disturbances in its availability may contribute to mood disorders linked with catatonic presentations.
The interplay between these metabolites and neurological functions highlights a complex relationship within the gut-brain axis. Exploring how specific compounds influence symptoms could pave the way for innovative therapeutic strategies targeting catatonia development.
Probiotics and Prebiotics: Potential Therapeutic Approaches
Probiotics and prebiotics are garnering attention for their potential role in managing catatonic states. Probiotics, which are live beneficial bacteria, can help restore a healthy balance of gut flora. This restoration may influence mood and behavior by enhancing the gut-brain communication pathway.
Prebiotics, on the other hand, serve as food for these good bacteria. They promote the growth of probiotics in the gut, helping to improve microbiome diversity. A diverse microbiome is essential for optimal brain function and overall mental health.
Studies suggest that certain strains of probiotics can reduce anxiety and depressive symptoms, which often accompany catatonia. By modulating neurotransmitter levels like serotonin and dopamine in the gut, they may positively impact emotional regulation.
Incorporating probiotic-rich foods or supplements could be an avenue worth exploring for individuals experiencing catatonic conditions. As research evolves, understanding how these elements interact with the gut-brain axis will become increasingly important in developing effective treatment strategies.
Dietary Factors Affecting the Gut-Brain Axis in Catatonia
Dietary factors play a crucial role in modulating the gut-brain axis, particularly in conditions like catatonia. A diet rich in fiber can promote a healthy microbiome, which is essential for maintaining gut health and overall well-being. Foods such as fruits, vegetables, and whole grains encourage the growth of beneficial bacteria that communicate with the brain.
Conversely, diets high in sugar and saturated fats may lead to dysbiosis—a microbial imbalance linked to various mental health issues. This imbalance can exacerbate symptoms associated with catatonia by negatively impacting neurotransmitter production.
Moreover, certain vitamins and minerals found in foods like leafy greens and nuts are vital for cognitive function. Deficiencies can impair neurotransmission processes necessary for emotional regulation.
Hydration also plays a key role; even mild dehydration can affect mood and cognitive clarity. Thus, dietary choices significantly influence the gut-brain connection and potentially impact catatonic states through this intricate relationship.
Stress, the Gut-Brain Axis, and Catatonic Presentations
Stress significantly impacts the gut-brain axis, influencing both mental and physical health. When individuals experience stress, their body enters a state of heightened alertness. This response can disrupt the delicate balance within the microbiome, potentially leading to dysbiosis.
Dysbiosis refers to an imbalance in gut bacteria that may exacerbate symptoms associated with catatonia. Research shows that chronic stress can lead to inflammation in the gut, which affects neurotransmitter production essential for maintaining mood and behavior. An altered microbial environment may further contribute to cognitive disturbances seen in catatonic states.
The connection between stress and gastrointestinal function also plays a role here. Stress triggers changes in digestive processes, affecting nutrient absorption vital for brain health. These changes could amplify feelings of lethargy or disconnection often observed during catatonia.
Moreover, prolonged exposure to stress can impair communication along the vagus nerve—an important pathway linking the gut and brain. Disruption of this communication signals potential pathways toward developing or worsening catatonic presentations.
Future Directions in Gut-Brain Axis Research for Catatonia
The exploration of the gut-brain axis in catatonic states opens up exciting avenues for future research. As we deepen our understanding, researchers are increasingly focusing on how specific gut microbiota can influence neurological health and mental disorders. There is a growing interest in identifying particular strains of probiotics that may mitigate symptoms associated with catatonia.
Innovative studies are examining the relationship between diet, gut health, and cognitive function. This includes investigating dietary interventions that could restore balance to the microbiome and potentially alleviate catatonic symptoms. Additionally, exploring genetic factors that affect individual responses to microbial therapies could lead to personalized treatment options.
Another promising area involves the development of biomarkers linked to dysbiosis or inflammation within the gut. These markers might provide insights into early detection and tailored treatment strategies for those at risk of developing catatonia.
As interdisciplinary collaboration increases among neurologists, psychiatrists, gastroenterologists, and nutritionists, we may unlock new therapeutic approaches leveraging the complex interplay between our gut health and brain function. Understanding how these systems interact will be crucial in advancing treatments for catatonic states and improving patient outcomes.


