Catatonia is a complex neuropsychiatric condition that can manifest in various ways, particularly through its motor symptoms. These symptoms range from peculiar body postures to disruptive and purposeless movements. Understanding the different types of motor symptoms associated with catatonia is crucial for early identification and effective treatment.
In this comprehensive guide, we will delve into the diverse spectrum of motor symptoms seen in catatonic patients. By shedding light on these characteristics, we aim to enhance awareness among caregivers, healthcare providers, and individuals experiencing these challenges. Whether you’re seeking knowledge for personal reasons or professional insight, this article will equip you with valuable information about the intricate world of catatonia’s motor manifestations.
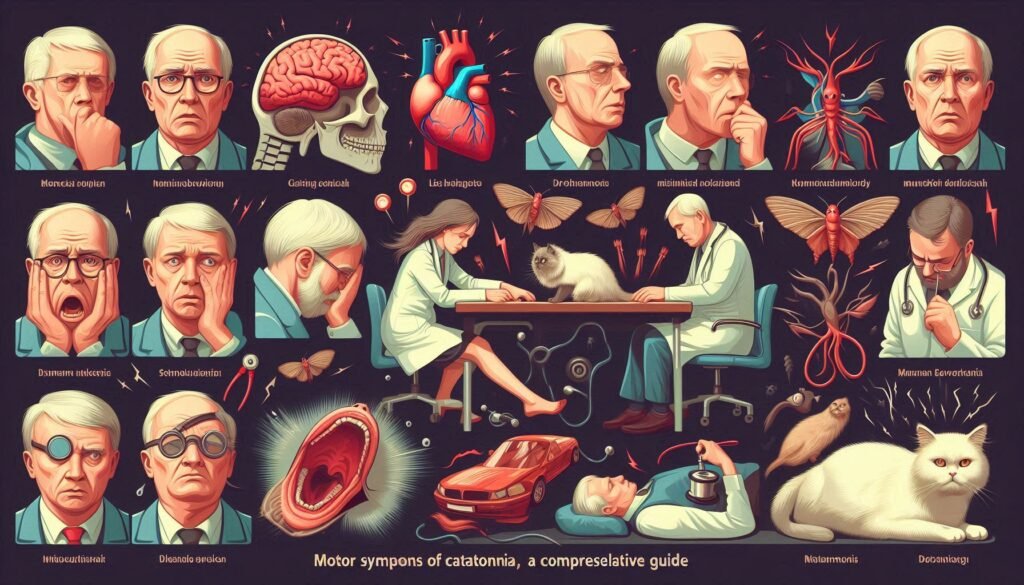
Overview of Motor Symptoms in Catatonia: Types and Characteristics
Motor symptoms of catatonia can be striking and varied, impacting individuals in different ways. These symptoms often fall into distinct categories that help healthcare providers identify the condition. Recognizing these types is essential for proper diagnosis and treatment.
One prominent type is catatonic immobility, where a person may exhibit stupor or rigidity, remaining fixed in a position for extended periods. This state can lead to physical complications if not addressed promptly.
On the opposite end of the spectrum lies catatonic excitement, characterized by excessive and purposeless motor activity. Individuals may display frantic movements without any clear intent or purpose during this phase.
Other notable motor characteristics include posturing—maintaining unusual body positions—and stereotypies involving repetitive gestures or actions. Each symptom provides critical clues about the underlying psychological state, making it vital to observe and report accurately for effective intervention.
Catatonic Immobility: Understanding Stupor and Rigidity
Catatonic immobility is a striking feature of catatonia, characterized by an inability to move or respond. Individuals may appear frozen in place, displaying stupor and rigidity. This state can last for extended periods, often leading to distressing situations for both the individual and their caregivers.
During stupor, a person may have a reduced level of awareness and responsiveness to external stimuli. They might not react even when stimulated physically or verbally. The absence of movement creates an unsettling atmosphere that can be alarming for loved ones observing the condition.
Rigidity manifests as stiffness in the body, making it difficult for individuals to change positions voluntarily. Muscles become tense and resistant to movement, which adds another layer of complexity when providing care.
Understanding these aspects is vital for recognizing catatonic symptoms early on. Prompt identification allows healthcare professionals to develop effective treatment plans tailored specifically to address motor abnormalities associated with this condition.
Catatonic Excitement: Excessive and Purposeless Motor Activity
Catatonic excitement is a striking motor symptom of catatonia characterized by excessive and often purposeless activity. Unlike typical restlessness, this condition manifests as frantic movements that may lack any clear intention or goal. Individuals experiencing catatonic excitement can seem agitated, performing repetitive actions such as pacing, hand-flapping, or even violent gestures.
This heightened state of movement can be distressing for both the person affected and those around them. The behaviors observed during catatonic excitement are not merely fidgeting; they may escalate to extreme agitation or even aggression in some cases. It’s essential to recognize these movements as part of a broader psychiatric issue rather than mere behavioral problems.
The experience can lead to physical exhaustion due to the continuous energy expenditure without relief. Observers might find it difficult to intervene effectively when someone is caught in this cycle of frenetic motion, making understanding crucial for better support.
Treatment often requires careful management strategies tailored specifically for individuals facing catatonic excitement. This approach helps ensure safety while addressing the underlying causes driving these intense motor symptoms.
Posturing and Catalepsy in Catatonia: Unusual Body Positions
Posturing and catalepsy are distinct yet interconnected motor symptoms observed in individuals experiencing catatonia. Posturing refers to the maintenance of abnormal body positions for an extended period, often regardless of discomfort or fatigue. Individuals may adopt unusual poses that can seem striking or bizarre.
Catalepsy is another phenomenon where a person maintains a rigid posture when placed in a specific position by someone else. This rigidity can last for several minutes to hours, indicating significantly altered muscle tone and responsiveness. It’s important to note that these states are not voluntary actions; they stem from underlying neurological disturbances.
Both posturing and cataleptic states highlight the profound impact of catatonia on motor control. These manifestations can sometimes lead to increased risk of injury due to falls or other accidents, emphasizing the need for careful monitoring during episodes.
Understanding these symptoms is crucial for proper diagnosis and treatment. Clinicians must recognize them as part of the broader spectrum of motor abnormalities linked with catatonia.
Stereotypies and Mannerisms: Repetitive Movements in Catatonia
Stereotypies and mannerisms are distinctive features of catatonia, characterized by repetitive and seemingly purposeless movements. These behaviors can manifest in various ways, such as hand flapping, rocking back and forth, or repeated facial grimaces. Although they may appear trivial to an observer, these actions often serve a crucial function for the individual experiencing them.
In many cases, stereotypies provide a sense of comfort or help alleviate anxiety during periods of heightened emotional distress. They can become ritualistic in nature—performed repeatedly without conscious thought. This repetition is not random; it reflects the brain’s attempt to process overwhelming stimuli.
Mannerisms differ slightly from stereotypies but share similar roots in abnormal motor behavior. Mannerisms might include exaggerated gestures or postures that seem out of context with the individual’s environment. Such movements can be socially isolating yet reveal underlying psychological struggles.
Understanding these repetitive movements is key for caregivers and healthcare professionals when assessing motor symptoms associated with catatonia. Proper evaluation helps inform treatment strategies aimed at improving patients’ quality of life.
Negativism and Automatic Obedience: Opposing Motor Behaviors
Negativism is a striking feature of catatonia, where individuals exhibit resistance to instructions or external stimuli. This can manifest as refusing to move, speak, or respond even when prompted. It may seem perplexing, but it plays a crucial role in understanding the complexity of motor symptoms associated with this condition.
On the other hand, automatic obedience presents an intriguing contrast. In this state, individuals comply effortlessly with commands without any conscious thought or awareness. For example, when asked to raise an arm, they may do so mechanically and without hesitation.
Both negativism and automatic obedience highlight the diverse spectrum of motor behaviors seen in catatonia. These opposing actions illustrate how deeply ingrained neurological processes influence behavior and response patterns in affected individuals.
Understanding these phenomena is essential for clinicians aiming to provide effective treatment strategies tailored to each patient’s unique presentation of motor symptoms associated with catatonia.
Echophenomena in Catatonia: Mimicking Movements and Actions
Echophenomena refer to involuntary imitation of movements, gestures, or actions observed in individuals with catatonia. This fascinating symptom highlights the complex interplay between motor control and psychological states. Those experiencing echophenomena might mimic another person’s behavior without conscious awareness.
This phenomenon can manifest as echolalia when it involves speech repetition or as simple gesture mimicry. It often occurs during moments of heightened emotional stress or sensory stimulation. The mimicking may appear bizarre but serves as an intriguing insight into the individual’s mental state.
Research suggests that these behaviors stem from disruptions in neural pathways responsible for voluntary movement and action perception. By echoing others, patients may be expressing their internal struggles or attempting to connect with their environment amid overwhelming feelings of disconnection.
Identifying echophenomena is essential for understanding the full spectrum of motor symptoms associated with catatonia. Clinicians can use this information to tailor treatment strategies that address both the behavioral aspects and underlying psychological factors contributing to this condition.
Assessment Tools for Catatonic Motor Symptoms
Assessing motor symptoms of catatonia is crucial for accurate diagnosis and treatment. Various standardized tools can help clinicians identify specific motor behaviors associated with this condition. One of the most commonly used assessment tools is the Bush-Francis Catatonia Rating Scale (BFCRS). This scale evaluates a range of motor symptoms, including immobility, posturing, and stereotypies.
Another effective tool is the Catatonia Assessment Scale (CAS), which focuses on quantifying different aspects of catatonic behavior. These assessments enable healthcare professionals to track changes in symptoms over time, guiding treatment decisions more effectively.
Clinicians may also use observational methods alongside these standardized scales to gather qualitative data about a patient’s behavior. This approach provides a comprehensive view of how catatonia manifests in each individual.
Early identification through thorough assessment enhances patient care significantly. Tailoring interventions based on precise evaluations helps improve outcomes for those experiencing motor symptoms associated with catatonia.
Treatment Approaches: Addressing Motor Abnormalities in Catatonia
Treatment for motor symptoms of catatonia typically involves a multi-faceted approach. The primary goal is to address the underlying causes while alleviating the specific motor abnormalities present in each individual. Early intervention can significantly improve outcomes.
Pharmacotherapy often includes benzodiazepines or antipsychotic medications, which may help reduce agitation and restore some level of normalcy in movement. Electroconvulsive therapy (ECT) is another effective treatment option, particularly for severe cases where rapid response is critical.
In addition to medication, supportive therapy plays a crucial role. Behavioral therapies can assist individuals in regaining control over their movements and reducing rigid posturing by employing gradual exposure techniques.
Collaborative care involving psychiatrists, neurologists, occupational therapists, and rehabilitation specialists ensures a comprehensive treatment plan tailored to the patient’s needs. This multidisciplinary strategy enhances recovery prospects by addressing both physiological and psychological aspects of catatonia.
Rehabilitation Strategies: Restoring Normal Motor Function
Rehabilitation is a crucial aspect of recovery for individuals experiencing motor symptoms of catatonia. An effective rehabilitation strategy focuses on restoring normal motor function and enhancing overall quality of life. It begins with thorough assessment and tailored interventions.
Physical therapy plays a significant role in addressing mobility issues caused by catatonic states. Therapists work to improve strength, coordination, and flexibility through targeted exercises that gradually build confidence and capability. Occupational therapy also helps patients regain independence in daily activities, encouraging engagement in tasks they may have abandoned during their illness.
In addition to physical modalities, psychological support is essential. Integrating psychotherapy can assist individuals in coping with the emotional effects of catatonia while promoting motivation for rehabilitation efforts. Mindfulness techniques can help reduce anxiety linked to movement difficulties.
Support from family members can further enhance the effectiveness of these strategies by fostering a nurturing environment where progress is celebrated—no matter how small it may seem at first. A multidisciplinary approach ensures all aspects are addressed comprehensively.
Restoring normal motor function requires patience, persistence, and collaboration among healthcare providers, patients, and families alike. With the right strategies in place, many individuals find hope not only in overcoming symptoms but also reclaiming their lives fully again.


