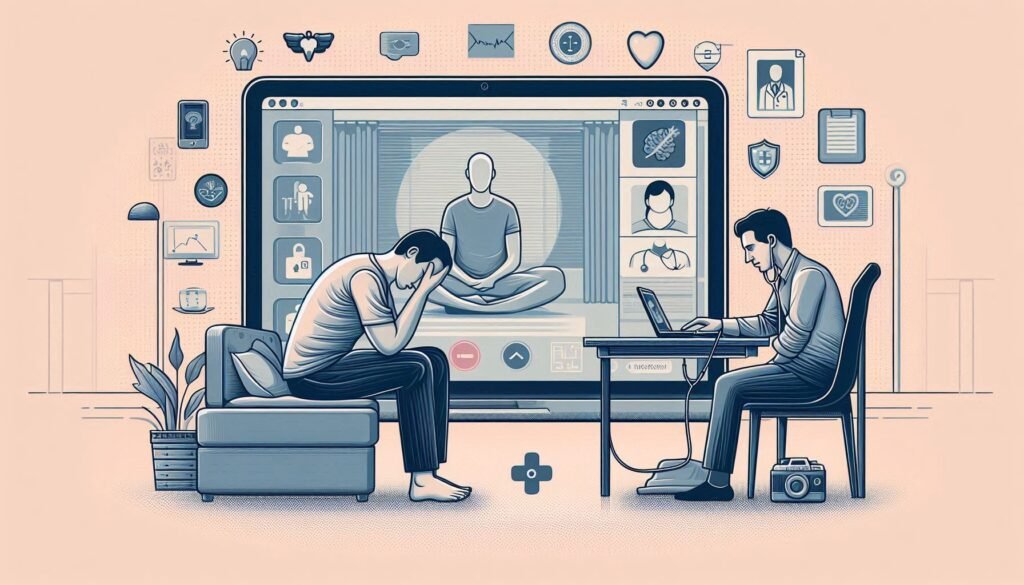
Telepsychiatry is revolutionizing the way mental health professionals connect with patients, especially when it comes to diagnosing complex conditions like catatonia. This remote approach offers a lifeline for patients who might otherwise struggle to access timely care. With its unique challenges and opportunities, telepsychiatry has become an essential tool in the psychiatrist’s toolkit.
Catatonic states can present a myriad of symptoms that often require nuanced observation and assessment. Traditional face-to-face evaluations can sometimes fall short due to accessibility issues or patient reluctance. However, leveraging technology allows clinicians to adapt their methods, ensuring comprehensive assessments are still possible from afar.
As we explore how telepsychiatry enhances the remote diagnosis of catatonic states, we’ll delve into everything from technical requirements and innovative interviewing techniques to caregiver involvement and ethical considerations. There’s much to learn about this evolving field that bridges distance while maintaining quality psychiatric care.
The Rise of Telepsychiatry: Opportunities and Challenges in Catatonia Diagnosis
Telepsychiatry has seen significant growth in recent years, particularly due to the demand for accessible mental health services. This rise is especially pertinent for diagnosing catatonic states, which can be challenging to identify without direct observation. Remote assessments allow patients who are homebound or living in underserved areas to receive timely care.
One of the key opportunities presented by telepsychiatry is flexibility. Clinicians can schedule appointments that fit their patients’ needs, leading to better engagement and adherence to treatment plans. Additionally, technology enables a broader reach, allowing specialists from various locations to contribute their expertise in catatonia diagnosis.
However, challenges remain. The lack of physical presence may hinder thorough examinations essential for identifying subtle signs of catatonia. Moreover, technical issues like poor internet connectivity can disrupt sessions and impact patient experience.
There’s also the consideration of privacy and data security concerns inherent in digital platforms used for remote consultations. Balancing these factors will be crucial as telepsychiatry continues evolving within psychiatric practice.
Setting Up for Success: Technical Requirements for Remote Catatonia Assessment
To effectively conduct remote assessments for catatonic states, a reliable technological setup is essential. High-speed internet access ensures stable video connections, minimizing interruptions during crucial evaluations. Both clinician and patient should ideally have devices with high-quality cameras and microphones to facilitate clear communication.
Choosing the right platform for telepsychiatry is also critical. HIPAA-compliant applications safeguard patient privacy while providing necessary functionalities for clinical interactions. Familiarity with these tools can ease the assessment process and enhance both parties’ comfort levels.
Lighting conditions matter too. A well-lit environment helps clinicians observe non-verbal cues that are vital in diagnosing catatonia accurately. Patients should be encouraged to sit in a space where their face is clearly visible to assist in this observational aspect.
Technical support must be readily available as well, addressing any issues swiftly so they don’t disrupt the session flow. This preparation sets the stage for effective remote diagnosis of catatonic states, allowing clinicians to deliver quality care regardless of physical distance.
Adapting Clinical Interviews for Virtual Catatonia Diagnosis
Adapting clinical interviews for virtual catatonia diagnosis requires careful consideration of both the medium and patient engagement. First, clinicians need to establish a rapport with the patient quickly. This can be achieved by creating an inviting virtual environment that fosters openness and trust.
Next, interviewers should adjust their questioning techniques. Open-ended questions encourage patients to share their experiences in detail. Focusing on specific symptoms such as mutism or abnormal posturing is crucial for accurate assessment.
Utilizing visual cues during video calls enables clinicians to observe non-verbal signs of catatonia effectively. Body language and facial expressions often provide valuable insights into the patient’s condition that might not be conveyed verbally.
Documenting responses meticulously remains essential in telepsychiatry settings. This ensures continuity of care while allowing for real-time adjustments to treatment plans based on ongoing assessments throughout the virtual interaction process.
Remote Physical Examination: Innovative Techniques for Assessing Catatonic Signs
Remote physical examinations present unique challenges when diagnosing catatonic states. However, innovative techniques are emerging to facilitate effective assessments through telepsychiatry. Clinicians can employ video consultations to observe patients’ body language and movements in real time, allowing for a preliminary evaluation of psychomotor symptoms.
One effective approach is the use of structured observation tools that guide clinicians on what specific signs to look for during remote sessions. These may include assessing posture, facial expressions, or abnormal motor activity using standardized assessment scales.
Additionally, caregivers can be trained to assist during virtual appointments. They can provide valuable insights into their loved ones’ behaviors while also demonstrating particular movements that indicate catatonic symptoms.
Utilizing technology like smartphone cameras enhances the ability to capture detailed visual data from multiple angles. This not only aids diagnosis but also helps track changes over time, making telepsychiatry an increasingly viable option in managing catatonia remotely.
Leveraging Technology: Digital Tools for Catatonia Symptom Tracking
Technology plays a vital role in modern telepsychiatry, particularly for tracking catatonia symptoms. Digital tools offer clinicians and caregivers the ability to monitor patient progress in real-time. These advancements facilitate timely interventions that can significantly improve patient outcomes.
Mobile applications dedicated to mental health provide symptom checklists tailored for catatonic states. Users can report their experiences daily, creating a comprehensive picture of their condition over time. This data becomes invaluable during remote consultations, allowing healthcare professionals to make informed decisions.
Wearable devices also contribute by monitoring physiological indicators like heart rate and movement patterns. Such continuous data collection helps detect subtle changes that may signal an escalation of symptoms or improvement.
Furthermore, secure cloud-based platforms enable seamless communication between patients and care teams. Sharing insights quickly fosters collaboration and ensures everyone involved is up-to-date on the patient’s status, enhancing the overall effectiveness of remote diagnosis efforts in catatonia management.
The Role of Caregivers in Remote Catatonia Assessment
Caregivers play a crucial role in the remote assessment of catatonic states. They are often the first to notice changes in behavior or mood, providing essential observational insights that can inform diagnosis. Their familiarity with the patient’s history and typical behaviors enhances the accuracy of assessments conducted via telepsychiatry.
During virtual consultations, caregivers help bridge communication gaps between patients and healthcare providers. They facilitate discussions by prompting patients to share their experiences and feelings, making it easier for professionals to gauge symptoms effectively. This collaboration is vital, as some individuals may struggle to articulate their condition during an episode.
Additionally, caregivers can assist in monitoring medication adherence and managing daily routines while providing emotional support. Their involvement ensures continuity of care even when direct supervision isn’t possible.
Empowered caregivers can also contribute valuable contextual information about environmental triggers or stressors that might exacerbate catatonic symptoms. This holistic approach enriches remote diagnosis efforts significantly.
Ensuring Patient Safety: Risk Assessment and Management in Virtual Settings
Ensuring patient safety in telepsychiatry is paramount, especially when diagnosing catatonic states. Risk assessment starts with a thorough understanding of the patient’s history. Clinicians must evaluate prior episodes, treatment responses, and any potential triggers for catatonia.
During virtual consultations, it’s crucial to identify warning signs that indicate worsening conditions or acute risks such as self-harm. Utilizing standardized assessment tools can help clinicians gather vital information about symptoms and behaviors that may not be immediately visible on screen.
Communication plays a key role in managing risk virtually. Establishing trust with patients encourages them to share concerns openly. Regular check-ins between appointments via phone calls or messaging can enhance monitoring and support.
Moreover, having an emergency protocol in place can safeguard against crises during remote sessions. This includes clear guidelines for contacting local emergency services if needed while ensuring caregivers are informed about their roles in supporting the patient’s safety at home.
Legal and Ethical Considerations in Telepsychiatric Catatonia Diagnosis
The legal and ethical landscape of telepsychiatry, particularly in diagnosing catatonic states, is complex. Practitioners must navigate varying state laws regarding the provision of mental health services across borders. Licensing requirements can differ significantly from one jurisdiction to another, necessitating careful attention to ensure compliance.
Informed consent becomes essential when delivering remote assessments. Patients should receive clear information about the nature of virtual consultations, potential limitations, and their rights. Transparency fosters trust and ensures that patients feel empowered during their treatment process.
Confidentiality is a critical concern as well. Telepsychiatric practitioners are obligated to safeguard patient information against breaches inherent in digital communications. Employing secure platforms for video calls and maintaining HIPAA compliance is vital in protecting sensitive data.
Ethical dilemmas may arise concerning the adequacy of remote diagnosis compared to traditional methods. Clinicians must weigh these challenges carefully while striving to provide effective care for those experiencing catatonic symptoms through telepsychiatric approaches.
Integrating Remote Assessments with In-Person Care for Catatonic Patients
The integration of remote assessments with in-person care can enhance the treatment journey for catatonic patients. Telepsychiatry allows healthcare providers to monitor symptoms regularly while ensuring that patients are comfortable in their familiar environments.
Remote evaluations offer flexibility, enabling clinicians to assess changes in behavior or symptoms quickly. Such timely insights can help inform decisions regarding immediate interventions or adjustments to treatment plans.
However, face-to-face interactions remain vital for a comprehensive evaluation of catatonia’s physical manifestations. In-person visits allow psychiatrists to conduct thorough examinations that may not be possible remotely, such as assessing motor responses and reflexes.
A hybrid model fosters collaboration between telehealth services and traditional care settings. This approach ensures continuity of care while leveraging the strengths of both modalities, ultimately providing better outcomes for patients experiencing catatonic states.
Future Directions: AI and Machine Learning in Remote Catatonia Diagnosis
The future of telepsychiatry and remote diagnosis of catatonic states is poised for transformation through the integration of artificial intelligence (AI) and machine learning. These technologies can enhance diagnostic accuracy by analyzing patterns in patient symptoms that may not be immediately apparent to clinicians. AI algorithms could sift through vast datasets, identifying correlations between specific behaviors and underlying psychiatric conditions.
Machine learning models can also improve real-time decision-making during virtual assessments. By continuously adapting based on new information, they offer personalized insights tailored to individual patients’ needs. This adaptability ensures a more nuanced understanding of catatonia’s complexities.
Additionally, incorporating AI-based tools into telepsychiatry platforms enables better tracking of symptom progression over time. Clinicians will have access to predictive analytics, which can inform treatment strategies before crises arise.
As we explore these innovations, it becomes clear that the combination of technology with traditional clinical practices holds great promise for improving outcomes in catatonic patients. By embracing digital advancements while maintaining human oversight, mental health professionals can create a more effective approach to diagnosing and managing this challenging condition remotely. The advancement toward an integrated model signifies hope for both practitioners and their patients navigating the intricate landscape of catatonia care.