Introduction to the Catatonia Symptom Spectrum: An Overview
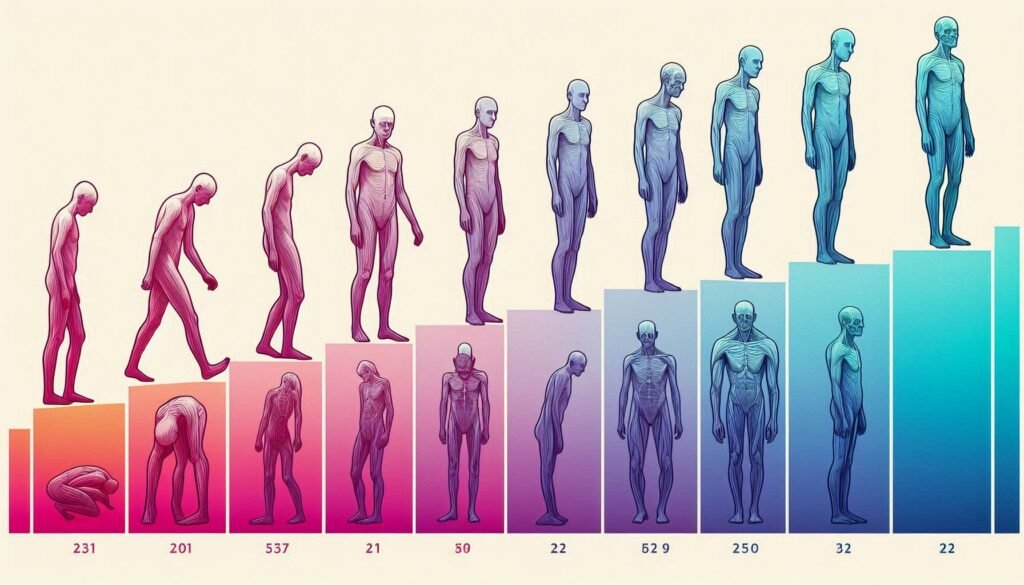
Catatonia is a complex and often misunderstood condition that manifests on a spectrum, ranging from mild to severe symptoms. While many people associate catatonia with complete immobility or unresponsiveness, the reality is far more nuanced. This mental state can present in subtle ways that might go unnoticed but still significantly impact daily life.
Understanding the full spectrum of catatonic symptoms is crucial for both patients and caregivers. It allows for earlier recognition and intervention, ultimately leading to better outcomes. Whether it’s slight rigidity in movements or profound emotional disturbances, each level has its own challenges and implications for treatment.
In this article, we will explore the various manifestations of catatonia—from the mildest signs to the most severe states—highlighting how they affect individuals differently. By shedding light on this spectrum, we aim to foster greater awareness and understanding about this often-overlooked aspect of mental health.
Mild Catatonic Symptoms: Subtle Signs and Their Impact
Mild catatonic symptoms can be quite subtle, often escaping the notice of those around the individual. These early signs may include slight motor agitation or decreased responsiveness to external stimuli. For instance, a person might appear less engaged in conversations or show limited facial expressions.
Another common indicator is a decline in social interaction. Friends and family may observe that the individual becomes withdrawn or shows little interest in activities they once enjoyed. This withdrawal can significantly impact relationships, leading to feelings of isolation.
Changes in speech patterns are also prevalent at this stage. Affected individuals might speak less frequently and offer short responses, making communication feel strained and challenging for both parties involved.
These mild symptoms shouldn’t be overlooked as they can evolve into more severe manifestations if left unaddressed. Early recognition is crucial for effective intervention and support before the condition escalates further. Addressing these subtleties can pave the way for better mental health outcomes.
Moderate Catatonia: Recognizing Escalating Symptoms
Moderate catatonia represents a crucial stage in the spectrum of catatonic symptoms. At this point, individuals may exhibit noticeable changes in behavior and motor functions. Unlike mild cases where signs are often subtle, moderate symptoms become more pronounced and harder to overlook.
Common indicators include increased rigidity or abnormal posturing. Individuals may adopt unusual positions for extended periods, reflecting an inability to initiate movement voluntarily. This can be distressing for both the individual and their caregivers, as it significantly impacts daily living activities.
Speech patterns also shift during this phase. People might experience reduced verbal output or respond only with brief phrases or single words. Such communication difficulties can lead to frustration and isolation from loved ones.
Cognitive challenges begin surfacing too; confusion over time, place, or even identity can occur. Recognizing these escalating symptoms is vital for timely intervention and support before they escalate further into severe manifestations of catatonia.
Severe Catatonic States: Extreme Manifestations and Risks
Severe catatonic states represent some of the most extreme manifestations of this complex condition. Individuals may exhibit profound motor disturbances, including complete immobility or rigidity. In these moments, they can remain in a fixed posture for hours or even days, unable to respond to external stimuli.
The risks associated with severe catatonia are significant. Prolonged immobility can lead to complications such as pressure sores and deep vein thrombosis. Additionally, individuals might experience malnutrition due to an inability or refusal to eat and drink.
Cognitive functions also decline sharply during severe episodes. This may include disorientation and an inability to engage in meaningful communication. The mental fog that accompanies severe catatonia can further exacerbate feelings of isolation.
Emotional responses often become muted or absent altogether. Those experiencing severe symptoms may appear emotionally flat, making it difficult for caregivers and loved ones to connect with them on any level.
Motor Symptoms Across the Spectrum: From Slight Rigidity to Complete Immobility
Motor symptoms in catatonia can vary significantly, ranging from slight rigidity to complete immobility. Mild cases may present as a subtle stiffening of the muscles. This rigidity might go unnoticed initially but can affect daily activities and posture.
As catatonia progresses, patients may exhibit more pronounced motor disturbances. Moderate symptoms often include unusual posturing or resistance to movement, making it difficult for caregivers to assist with basic tasks. These changes can lead to frustration for both the individual experiencing them and those around them.
In severe forms of catatonia, individuals may become completely immobile or exhibit waxy flexibility—where limbs remain in whatever position they are placed by others. This state poses significant challenges for treatment and care.
The impact on physical health is profound when mobility decreases dramatically. Risks such as pressure sores and respiratory issues increase substantially during severe episodes. Understanding these motor symptoms is crucial in identifying appropriate interventions early on.
Speech and Communication: The Progression from Reduced Verbalization to Mutism
Speech and communication are integral components of human interaction, yet catatonia can drastically alter these abilities. Individuals at the mild end of the spectrum may experience reduced verbalization, where speech becomes less frequent or more hesitant. This subtle change can often go unnoticed by those around them but significantly impacts their ability to engage socially.
As symptoms progress into moderate catatonia, individuals might demonstrate even further declines in communication skills. They may respond only with short phrases or monosyllabic answers. The emotional connection once present in conversations starts to fade as the person withdraws from social exchanges.
At the severe end of the spectrum lies mutism—a complete lack of verbal response. In this state, individuals may appear unresponsive and disconnected from their surroundings. This absence of speech is not merely a choice; it’s often a symptom rooted deeply in their condition.
Understanding these variations is crucial for caregivers and loved ones when recognizing changes that could indicate worsening symptoms within the spectrum of catatonic symptoms.
Cognitive Symptoms: Mild Confusion to Severe Thought Disturbances
Cognitive symptoms in catatonia manifest on a spectrum, beginning with mild confusion. Individuals may struggle to concentrate or experience fleeting moments of forgetfulness. These subtle changes can often be overlooked but are significant indicators of underlying issues.
As the severity increases, cognitive disturbances can become more pronounced. Patients might exhibit disorganized thinking, making it challenging to follow conversations or stay engaged in tasks. This level of impairment affects their daily functioning and social interactions.
In severe cases, thought processes can distort dramatically. Some individuals may experience delusions or hallucinations, leading to profound disconnection from reality. These disruptions create an environment where rational decision-making becomes nearly impossible.
Such cognitive challenges not only affect personal relationships but also complicate treatment plans. Recognizing these symptoms early is vital for effective intervention and support systems tailored to each individual’s needs within the spectrum of catatonic symptoms.
Emotional and Behavioral Changes: Across the Catatonia Spectrum
Emotional and behavioral changes represent a crucial aspect of the spectrum of catatonic symptoms. Individuals may experience varied emotional responses, ranging from mild anxiety to profound despair. These fluctuations can significantly impact their daily lives and social interactions.
In mild cases, individuals might appear withdrawn or display reduced interest in activities they once enjoyed. This subtle shift can be easily overlooked but is essential for early detection. As severity increases, behaviors can escalate to agitation or even extreme irritability.
Moderate catatonia can lead to more pronounced emotional disturbances. These individuals may exhibit erratic moods, oscillating between periods of heightened emotion and complete detachment from their surroundings. The unpredictability becomes distressing not only for them but also for loved ones trying to provide support.
In severe cases, emotional expression often diminishes drastically. Individuals may present with flat affect or become entirely unresponsive emotionally. Such profound changes highlight the urgent need for appropriate intervention tailored to each symptom’s severity on this complex spectrum.
Physical Health Risks: How Severity Impacts Overall Wellbeing
Catatonia can have significant implications for physical health, particularly as symptoms escalate. In mild cases, individuals may experience reduced mobility or changes in appetite, which might seem manageable at first. However, these subtle shifts can gradually lead to more serious issues if left unaddressed.
As catatonic symptoms become moderate to severe, risks increase substantially. Prolonged immobility can result in muscle wasting and joint problems. Additionally, patients may develop pressure sores due to lack of movement. These complications not only affect comfort but also overall mobility.
Severe catatonia often leads to a total inability to care for oneself. This decline raises the risk of malnutrition and dehydration since basic needs go unmet. The longer someone remains in this state, the greater the potential for life-threatening conditions.
Moreover, extreme emotional distress associated with severe catatonia can impact cardiovascular health. Stress hormones may rise significantly during episodes of heightened anxiety or agitation that accompany these states.
Treatment Approaches: Tailoring Interventions to Symptom Severity
Understanding the spectrum of catatonic symptoms is essential for effective treatment. Each level—mild, moderate, and severe—demands a unique approach tailored to the individual’s needs. For mild symptoms, interventions may include psychotherapy or lifestyle adjustments that focus on stress management and social engagement.
As symptoms escalate to moderate levels, medication can become crucial. Antipsychotics or benzodiazepines might be administered to alleviate distressing manifestations while providing supportive therapy aimed at restoring communication and cognitive function.
Severe catatonia often requires more intensive intervention. Hospitalization may be necessary for patient safety and stabilization. In these cases, electroconvulsive therapy (ECT) has proven effective in rapidly addressing acute symptoms.
Moreover, continuous monitoring of physical health risks is vital across all severity levels. Early detection leads to timely medical assessments that safeguard overall well-being during treatment.
Collaboration among healthcare providers is key when developing a comprehensive care plan that addresses both psychological and physical aspects of catatonia based on its symptom spectrum.


