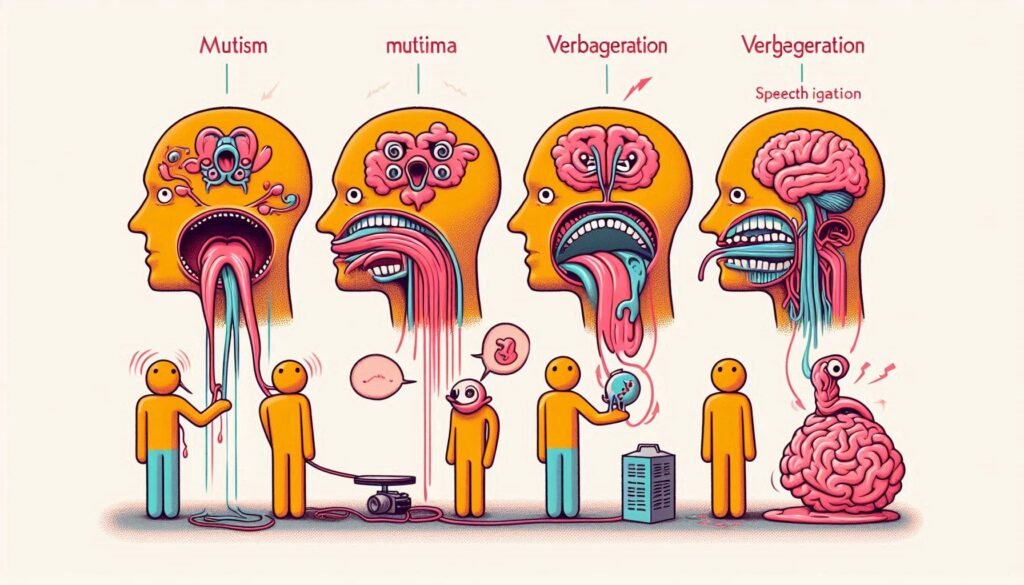
Catatonia is a complex neuropsychiatric condition that significantly impacts communication. One of the most fascinating yet challenging aspects of catatonia is its array of speech patterns, which can range from complete silence to repetitive verbalizations. Understanding these diverse manifestations provides crucial insights for caregivers and healthcare professionals alike.
Whether it’s the sudden onset of mutism or the echoing phrases characteristic of verbigeration, each speech pattern in catatonia tells a story about the individual’s mental state. These variations not only reflect underlying neurological processes but also influence how we approach treatment and care strategies.
In this article, we will explore the spectrum of speech patterns in catatonia, shedding light on their implications for diagnosis, communication barriers faced by patients, and effective treatment options available today. Join us as we delve into this intricate world where words may be absent or endlessly repeated, offering a deeper understanding of those affected by catatonia.
Understanding the Range of Speech Patterns in Catatonia
Catatonia is characterized by a variety of speech patterns that can profoundly affect communication. These patterns are not merely random but often reflect underlying psychological and neurological states. From mutism to echolalia, the spectrum of speech behaviors offers vital clues into an individual’s condition.
Each patient may exhibit different manifestations of catatonia, which complicates diagnosis and treatment. Some individuals may become completely silent, while others engage in repetitive or imitative speech. The presence or absence of verbal communication can influence how caregivers interact with these patients.
Additionally, the context surrounding each patient’s experience plays a crucial role in their expression. Stressors such as hospitalization or changes in routine may exacerbate specific speech patterns. Understanding this range aids healthcare professionals in crafting tailored approaches for care.
Recognizing these diverse symptoms allows both clinicians and families to better support affected individuals. Awareness fosters empathy and improves interactions, ultimately enhancing the quality of care provided to those experiencing catatonic conditions.
Catatonic Mutism: When Silence Dominates
Catatonic mutism is a profound state characterized by an absence of verbal communication. Individuals experiencing this condition may appear alert but remain unresponsive to external stimuli. The silence can be striking, often leading caregivers and family members to feel helpless in their attempts to engage the affected person.
During episodes of catatonic mutism, individuals might maintain eye contact or exhibit minimal physical movements. However, they do not respond verbally or even nod in acknowledgment. This lack of communication can create significant challenges for both the individual and those around them.
The duration of catatonic mutism can vary greatly—from hours to days or even longer. Understanding that this behavior is rooted in a neurobiological condition rather than intentional defiance is crucial for supporting affected individuals compassionately.
Various underlying factors contribute to catatonic mutism, including mood disorders, schizophrenia, or neurological conditions. Recognizing these associations helps healthcare providers tailor appropriate interventions aimed at restoring communication and engagement over time.
Verbigeration: Repetitive Speech in Catatonic States
Verbigeration is a fascinating phenomenon observed in individuals experiencing catatonia. It refers to the involuntary repetition of certain words or phrases, often devoid of context or meaning. This behavior can be distressing and confusing for both the individual and those around them.
In many cases, verbigeration manifests as persistent utterances that may seem nonsensical. These repetitions are not simply random; they reflect an underlying neurological disturbance associated with catatonic states. The repeated speech can vary from single words to complex phrases, occurring at different frequencies.
The presence of verbigeration highlights the unique relationship between speech patterns and mental health conditions like catatonia. Understanding this repetitive speech pattern can provide insights into the emotional state and cognitive processes of affected individuals.
Interventions focusing on communication techniques might assist caregivers in managing interactions with someone exhibiting verbigeration. Recognizing when these patterns occur enables better support for those navigating such challenging experiences.
Echolalia in Catatonia: Mimicking Others’ Speech
Echolalia is a fascinating phenomenon often observed in catatonic states. It involves the involuntary repetition of phrases or words spoken by others. This behavior can manifest as an immediate response or after a delay, depending on the individual’s condition.
In catatonia, echolalia serves different functions. For some individuals, it acts as a way to engage with their environment when initiating conversation feels overwhelming. Mimicking speech may provide comfort and familiarity in moments of distress.
Interestingly, echolalic responses can vary widely among patients. Some might repeat entire sentences verbatim while others select specific phrases that resonate with them emotionally or contextually. This variability highlights the complexity of communication within catatonic disorders.
Understanding echolalia is crucial for caregivers and clinicians alike. By recognizing this speech pattern, they can adapt their communication strategies to foster engagement and support recovery efforts effectively.
Prosody and Intonation Changes in Catatonic Speech
Prosody and intonation play crucial roles in human communication. In catatonia, these elements often become markedly altered. Patients may display a monotone voice, lacking the usual variations in pitch and rhythm that convey emotion or emphasis.
This flatness can lead to misunderstandings during interactions. Listeners might struggle to gauge the speaker’s feelings or intentions due to the absence of vocal nuances. Such changes can make conversations feel robotic or detached, further isolating individuals affected by catatonia.
Additionally, some patients may exhibit exaggerated prosodic features at times. This inconsistency complicates their ability to communicate effectively. Speech may fluctuate between overly emphatic delivery and complete lack of modulation.
Understanding these shifts is vital for caregivers and healthcare professionals. Recognizing the nature of prosodic changes helps improve interaction strategies with those experiencing speech disturbances related to catatonia.
The Neurobiology of Speech Disturbances in Catatonia
Catatonia is a complex neuropsychiatric condition that affects speech patterns significantly. The underlying neurobiology involves multiple brain regions, including the basal ganglia and frontal cortex, which play crucial roles in motor control and language processing. Dysfunction in these areas can lead to disruptions in both voluntary movement and verbal communication.
Neurotransmitters such as dopamine and gamma-aminobutyric acid (GABA) are essential for regulating mood and behavior. In catatonic states, imbalances in these chemicals may contribute to phenomena like mutism or verbigeration. For instance, reduced dopamine activity can hinder motivation to speak.
Furthermore, structural changes within the brain may be observed through imaging techniques. These abnormalities often correlate with specific speech disturbances seen in patients experiencing catatonia. Understanding this neurobiological foundation helps clinicians better identify symptom patterns.
Research into these disturbances continues to evolve. By uncovering the intricate links between neural pathways and speech behaviors, new therapeutic avenues may emerge aimed at improving outcomes for individuals affected by catatonia.
Assessing Speech Patterns: Diagnostic Tools and Techniques
Assessing speech patterns in catatonia requires a comprehensive approach. Clinicians often utilize structured interviews to gather detailed patient histories. These interviews can reveal the onset and duration of speech abnormalities, which are crucial for diagnosis.
Standardized assessment tools play a vital role as well. Instruments like the Positive and Negative Syndrome Scale (PANSS) help evaluate various symptoms associated with schizophrenia, including catatonia. This allows healthcare providers to quantify changes over time effectively.
Observational techniques are also essential during assessments. Caregivers may note specific behaviors such as mutism or verbigeration in different settings. This information aids clinicians in understanding how these speech patterns affect daily life.
Collaboration among multidisciplinary teams is beneficial too. Psychiatrists, psychologists, and speech therapists can work together to create a holistic picture of the patient’s condition, ensuring that all aspects of their communication difficulties are addressed appropriately.
Impact of Speech Abnormalities on Communication and Care
Speech abnormalities in catatonia can significantly hinder effective communication. Individuals may struggle to convey their thoughts or needs, leading to frustration and isolation. This silence can create a gap between patients and caregivers, making it challenging for both parties to understand each other.
Moreover, these speech disturbances often affect the emotional well-being of those experiencing them. The inability to express oneself verbally can lead to feelings of helplessness or despair. Caregivers might misinterpret behavior as disinterest rather than recognizing the underlying condition affecting communication.
In therapeutic settings, understanding speech patterns becomes essential for tailored care strategies. Acknowledging variations like mutism or verbigeration helps professionals adapt their approaches accordingly. This ensures that interventions are both compassionate and effective.
Additionally, enhancing non-verbal communication methods is crucial in supporting individuals with catatonia. Gestures, facial expressions, and visual aids can bridge the communicative divide and foster connection while respecting the unique challenges presented by speech abnormalities.
Treatment Approaches: Addressing Speech Issues in Catatonia
Treatment approaches for addressing speech issues in catatonia often require a multidisciplinary strategy. Mental health professionals, including psychiatrists and speech-language pathologists, work together to create effective treatment plans tailored to individual needs. Medication plays a crucial role; antipsychotics or benzodiazepines may help alleviate symptoms that hinder communication.
Psychotherapy can also be beneficial, particularly when incorporating cognitive-behavioral techniques. These methods focus on building rapport with the patient and encouraging gradual engagement in conversation. The therapeutic environment must be supportive and non-threatening to foster communication.
Speech therapy is essential for patients experiencing mutism or other speech abnormalities. Techniques such as modeling appropriate speech patterns and using visual aids can aid recovery. Gradual exposure to verbal interactions helps reestablish confidence in their ability to communicate effectively.
Family involvement is critical during this process. Educating loved ones about catatonia promotes understanding and patience while facilitating open lines of communication within the support network.
Recovery of Speech Function: What to Expect and How to Support
Recovery of speech function in individuals experiencing catatonia can be a gradual and nuanced process. Each person’s journey is unique, influenced by the severity of their condition and underlying factors such as mental health history. Expect fluctuations in communication abilities during recovery; some may regain their ability to speak quickly, while others might require more time.
Support plays a pivotal role in this recovery phase. Creating a safe, nurturing environment encourages open expression without pressure or judgment. Engaging with speech-language pathologists can provide tailored strategies that cater to individual needs, enhancing both verbal and non-verbal communication skills.
Implementing consistent routines offers stability that many find reassuring amidst cognitive challenges. Patience is key; celebrate small milestones along the way as they signify progress.
Family members and caregivers should educate themselves on catatonia’s complexities to foster understanding and empathy throughout this journey. Encouragement combined with professional guidance fosters an atmosphere conducive to healing. Every step taken towards renewed speech is a testament to resilience—both for those affected and their support networks.


