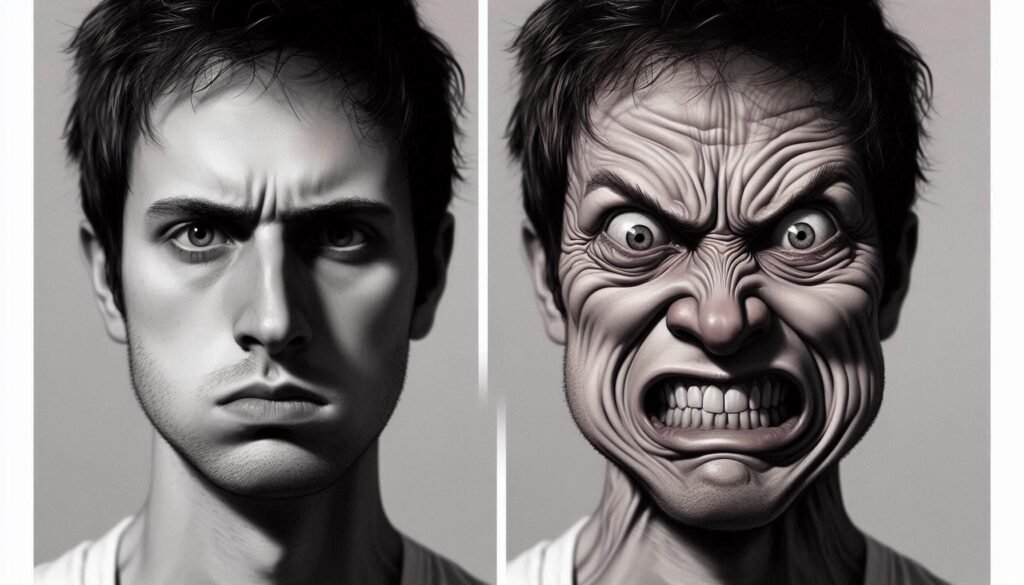
Catatonia is a complex neuropsychiatric condition that often manifests through notable physical symptoms, particularly facial expressions. Among these, staring and grimacing can be perplexing yet revealing signs of an underlying disorder. For families and caregivers navigating the challenges posed by catatonic patients, understanding these facial expressions becomes crucial.
Staring may suggest a dissociation from reality, while grimacing could indicate distress or discomfort. Both behaviors not only affect patient communication but also provide vital clues about their mental state. As we delve deeper into the characteristics and significance of these expressions, you’ll discover how they serve as windows into the cognitive processes of those experiencing catatonia.
Join us on this journey to unravel the mysteries behind staring and grimacing in catatonic patients—an exploration that promises insights for better care and support strategies for individuals affected by this challenging condition.
Understanding Catatonic Staring: Characteristics and Significance
Catatonic staring is a prominent feature often observed in individuals affected by catatonia. This behavior typically presents as a prolonged, unblinking gaze directed at an object or space. The intensity and duration of the stare can vary widely among patients.
The significance of this expression goes beyond mere observation. It often signifies a dissociative state where the individual appears disconnected from their surroundings. This disengagement can stem from an overwhelming emotional experience, anxiety, or neurological dysfunction.
Understanding these characteristics helps healthcare providers assess patient needs more accurately. Staring may indicate that the patient is experiencing distress or simply unable to process stimuli in their environment effectively.
Recognizing catatonic staring also fosters better communication strategies for caregivers. By being aware of when patients are engaged in this state, caregivers can tailor their approaches to offer appropriate support and reassurance without adding further stress to the situation.
Grimacing in Catatonia: Types and Clinical Importance
Grimacing in catatonia can manifest in various forms, each serving as a significant clinical indicator. These facial expressions often reflect underlying distress or discomfort that may not be verbalized due to the patient’s condition. The types of grimaces can range from slight furrowing of the brow to more pronounced contortions involving the mouth and eyes.
Certain grimaces might indicate specific psychological states or reactions to stimuli. For example, a patient may exhibit a scowl when experiencing agitation. Conversely, a blank stare combined with minimal facial movement might denote withdrawal or depression.
Understanding these variations is crucial for healthcare providers as they assess treatment needs and responses. Grimacing not only aids in diagnosing catatonic episodes but also helps differentiate between different psychiatric disorders.
Recognizing grimacing patterns allows caregivers to tailor interventions effectively. This enhances communication strategies and ensures that support aligns with patients’ emotional and physical experiences during their care journey.
The Neurology Behind Catatonic Facial Expressions
Catatonia is a complex neuropsychiatric syndrome often characterized by distinct facial expressions, including staring and grimacing. The neurological basis behind these manifestations involves disruptions in various brain circuits. Specifically, the basal ganglia plays a crucial role in regulating motor control, which can lead to abnormal postures and facial movements.
Dopaminergic pathways are also implicated in catatonic states. An imbalance of dopamine neurotransmission may contribute to the rigidity and immobility witnessed in patients. This dysregulation affects not only voluntary movement but also involuntary responses that result in specific facial expressions.
Moreover, studies suggest that altered connectivity between areas like the prefrontal cortex and other regions could explain why some individuals display fixed stares or exaggerated grimaces. These neural disturbances prevent effective communication through typical non-verbal cues.
Understanding this neurology helps caregivers better interpret the behaviors of catatonic patients. Recognizing that these facial expressions stem from underlying brain dysfunction sheds light on their clinical significance.
Differentiating Catatonic Facial Symptoms from Other Conditions
Differentiating catatonic facial symptoms from other conditions is vital for accurate diagnosis and treatment. Catatonia often features distinctive expressions, such as staring and grimacing, which can be mistaken for signs of neurological disorders or mood disturbances. Conditions like Parkinson’s disease may also present with similar facial rigidity but differ in underlying causes.
For instance, patients experiencing dystonia might show abnormal postures or movements that are not typically seen in catatonia. Understanding these nuances requires careful observation by healthcare professionals. A thorough clinical evaluation can help discern the specific type of motor disturbance.
Additionally, schizophrenia-related catatonia has unique characteristics that set it apart from other psychiatric conditions. Symptoms may include a lack of emotional expression paired with unresponsiveness, distinct from depressive episodes where sadness prevails.
Accurate differentiation hinges on recognizing patterns within facial expressions and accompanying behaviors. This approach aids clinicians in developing appropriate interventions tailored to each patient’s needs without misdiagnosis or delay in care.
Impact of Staring and Grimacing on Patient Communication
Staring and grimacing are common facial expressions seen in catatonic patients. These manifestations can significantly impact communication between the patient and their caregivers. When a patient stares blankly, it often creates a barrier that hinders understanding and interaction.
Grimacing, on the other hand, may convey distress or discomfort. Caregivers need to interpret these non-verbal cues accurately. Misinterpretation can lead to feelings of frustration for both parties involved.
The lack of verbal communication complicates matters further. Patients may struggle to express needs or emotions verbally due to their condition. This silence amplifies reliance on facial expressions as primary communicative tools.
Understanding these nuances is essential for effective care. By recognizing staring and grimacing as significant forms of expression, caregivers can better respond to patients’ emotional states and needs, fostering a more supportive environment for recovery.
Assessing Severity: How Facial Symptoms Reflect Overall Catatonic State
Assessing the severity of catatonia involves careful observation of facial symptoms, particularly staring and grimacing. These expressions can indicate the intensity of a patient’s condition. For instance, prolonged staring may suggest an acute state where the patient is disengaged from their environment.
Grimacing often reflects distress or discomfort, signaling that deeper psychological issues might be at play. The frequency and duration of these facial manifestations can provide vital clues about a patient’s mental status and level of responsiveness.
Clinicians utilize standardized scales to evaluate catatonic features alongside facial expressions for more comprehensive assessments. This approach helps in determining treatment plans tailored to each individual.
Moreover, changes in facial expressions over time are critical indicators of progress or decline in therapy outcomes. Regular monitoring allows healthcare providers to adjust interventions as needed based on observable behavioral cues.
Treatment Approaches: Addressing Facial Manifestations in Catatonia
Treatment for facial manifestations in catatonic patients requires a multifaceted approach. Psychotropic medications are often the first line of defense. Benzodiazepines and antipsychotics can help reduce symptoms such as staring and grimacing, allowing for improved communication.
Psychotherapy also plays a vital role. Techniques like cognitive-behavioral therapy may provide insights into emotional triggers behind these expressions. A supportive therapeutic environment encourages patients to express feelings non-verbally, reducing anxiety associated with their condition.
Physical interventions can be beneficial too. Occupational therapy focuses on motor skills that might alleviate some involuntary movements or facial rigidity. This holistic strategy aims to enhance overall functioning by addressing both psychological and physical aspects of catatonia.
Collaboration among healthcare providers is essential for optimal care delivery. Regular assessments allow caregivers to adjust treatment plans according to the patient’s evolving needs, ensuring that all facets of their well-being are considered during recovery efforts.
The Role of Non-Verbal Communication in Catatonic Patient Care
Non-verbal communication plays a vital role in the care of catatonic patients. Due to their limited verbal responses, facial expressions become essential tools for understanding their needs and emotions. Caregivers often rely on these non-verbal cues to gauge pain levels, discomfort, or anxiety.
Observing subtle changes in facial expressions can provide insights into a patient’s mental state. For instance, slight shifts from staring to grimacing may indicate distress or an emerging need for intervention. Recognizing these signals helps caregivers respond more effectively.
Moreover, maintaining eye contact can foster a sense of connection with catatonic patients. Even if they do not reciprocate verbally, this form of engagement reassures them that someone is present and attentive to their well-being.
In therapeutic settings, encouraging expression through gestures or visual aids enhances communication further. This approach ensures that even those who cannot articulate feelings still receive empathetic support tailored to their unique experiences.
Family and Caregiver Guidance: Interpreting Facial Cues in Catatonia
Understanding facial cues in catatonic patients can be challenging for families and caregivers. Catatonia often presents with staring and grimacing, which may not convey the usual emotional states we associate with these expressions. Recognizing that these manifestations are part of a broader clinical picture is crucial.
Families should learn to observe their loved one’s behavior closely. A prolonged stare might signify deep concentration or withdrawal rather than mere disinterest. Similarly, grimacing could reflect discomfort or anxiety, which the patient may not be able to verbally express.
Effective communication is vital. Caregivers can try speaking softly and maintaining eye contact when engaging with someone exhibiting these symptoms. This approach fosters a sense of connection despite the lack of verbal interaction.
Additionally, keeping a journal detailing facial expressions alongside other behaviors can help healthcare providers tailor interventions more effectively. It empowers families by providing insights into patterns that may emerge over time.
Long-Term Management and Prognosis of Facial Symptoms in Catatonia
Long-term management of facial symptoms in catatonia requires a comprehensive approach. Continuous assessment is vital for understanding how staring and grimacing evolve over time. Regular monitoring helps identify changes that may indicate worsening or improvement of the patient’s condition.
Therapeutic interventions often focus on both pharmacological and psychosocial strategies. Medications, such as antipsychotics or benzodiazepines, can be effective in alleviating severe symptoms. Alongside medication, supportive therapies play a crucial role. Occupational therapy and speech-language pathology can help improve non-verbal communication skills.
Family involvement is essential for fostering better outcomes. Caregivers should be educated about recognizing facial cues, which can enhance their ability to respond appropriately to patients’ needs. This education also aids families in creating a supportive environment that encourages emotional expression and connection.
Prognosis varies widely among individuals with catatonia. Some may experience significant improvements with treatment, while others might face challenges due to persistent symptoms like staring and grimacing. Early intervention remains key; it often leads to more favorable long-term results.
By focusing on tailored care plans and ongoing support systems, healthcare providers can significantly influence the trajectory of facial expressions in catatonic patients—ultimately improving their quality of life.


